A sudden bright-red patch on the white of your eye can be startling. It looks dramatic, almost like a scene out of a thriller, but in most cases, it’s no big deal. What you’re seeing is usually a broken blood vessel, or what doctors call a subconjunctival hemorrhage. It often clears on its own within one to three weeks. Still, sometimes that splash of red is more than just cosmetic.
Most Common Causes of Broken Blood Vessels in the Eye
Strong coughing or sneezing — 30%
A sudden pressure spike in the chest and head forces fragile eye capillaries to burst.
Eye trauma — 20%
Accidents like rubbing with a nail or flying debris during work can directly injure eye vessels.
High blood pressure — 25%
Constant elevated pressure weakens small vessels, making them prone to rupture.
Post-surgery complications — 10%
Procedures like LASIK or cataract surgery may leave small surface bleeds from suction or strain.
Blood-thinning drugs or supplements — 15%
Warfarin, aspirin, or ginkgo reduce clotting, so even minor strain can trigger visible bleeding.
Source: eyexan.com
This article breaks down the causes, symptoms, risks, and modern treatment options — along with expert commentary from medical consultant Reyus Mammadli — so you’ll know when to relax and when to pick up the phone for a doctor’s appointment.
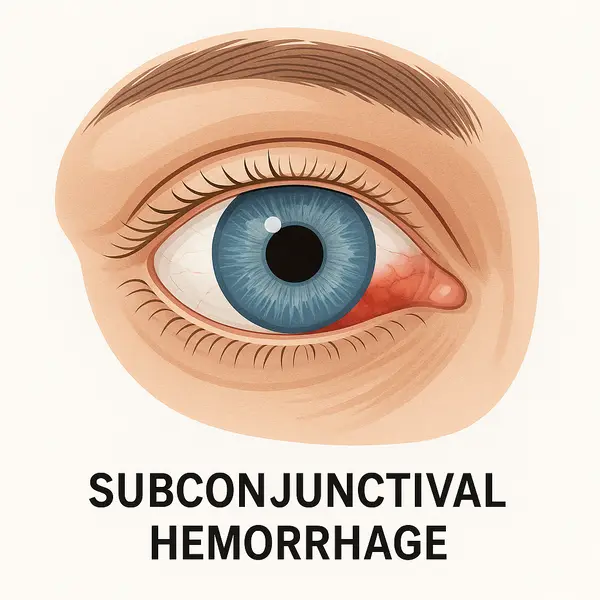
What Is a Broken Blood Vessel in the Eye?
A broken blood vessel in the eye, medically called a subconjunctival hemorrhage, occurs when one of the tiny capillaries under the conjunctiva (the thin, clear tissue that covers the sclera) ruptures. The trapped blood spreads out, creating a sharply defined red patch. Despite the shocking look, the condition is usually harmless and doesn’t affect vision.
According to the American Academy of Ophthalmology, about 2–3% of adults in the United States experience at least one subconjunctival hemorrhage during their lifetime ⧉. Most cases resolve without treatment in 7–14 days, though some may last up to three weeks.
Unlike conjunctivitis or infections, a subconjunctival hemorrhage doesn’t cause discharge, swelling, or itching. Many people discover it by chance in the mirror or when a friend points it out.
Common Causes of Broken Blood Vessels in the Eye
A subconjunctival hemorrhage may seem random, but most of the time there’s a clear reason behind it. Understanding these everyday triggers, medical factors, and lifestyle contributors makes it easier to know which are harmless and which may need a doctor’s attention. Each cause below is explained with practical examples and a quick take on how serious it is.
Sudden Pressure Changes
Even simple actions can spike pressure in the tiny vessels of your eye. A strong sneeze during allergy season, a deep cough from bronchitis, or straining on the toilet can be enough to make a fragile vessel pop. Think of it like over‑inflating a balloon until one weak spot bursts. Seriousness: Usually mild; clears on its own.
Eye Trauma
Direct injury can cause broken vessels. This might be accidental — rubbing your eye too hard with a fingertip or scratching it with a nail, or when a wood chip or speck of metal flies in while working in a garage. Contact sports without protective eyewear are another common scenario. Here the blood vessel rupture is the eye’s version of a bruise after bumping your shin. Seriousness: Can range from mild to severe depending on the force; trauma always deserves an eye exam.
Post-Surgery Changes
After vision procedures like LASIK or cataract surgery, subconjunctival hemorrhages often appear. Suction rings, surgical instruments, or even the act of straining too soon after surgery can leave a red patch. It’s similar to seeing a small bruise near a surgical incision on the skin. Seriousness: Usually mild and expected; still, surgeons monitor healing closely to rule out complications.
Chronic Health Conditions
High blood pressure and diabetes weaken small vessels over time. Imagine old pipes that become brittle — under pressure they’re more likely to leak. Repeated subconjunctival hemorrhages in these patients may be the first sign their underlying condition isn’t controlled. Seriousness: Significant; medical evaluation required.
Medications and Supplements
Blood thinners like warfarin, aspirin, clopidogrel (Plavix) and high‑dose supplements such as vitamin E or ginkgo biloba reduce the blood’s ability to clot. Even a light cough can then trigger bleeding on the eye’s surface. Seriousness: Variable; often harmless, but repeated cases need medication review ⧉.
Emotional Stress and Tears
Intense crying or prolonged stress doesn’t just affect mood — the physical act of squeezing eyelids tightly or raising blood pressure can sometimes burst a vessel. Picture clenching your fists so hard your knuckles turn white; the same physical strain can happen in the eyes. Seriousness: Usually mild; self‑resolving.
Editorial note: Reyus Mammadli emphasizes that while many causes are harmless, trauma, repeated hemorrhages, or those linked to systemic disease always warrant a professional exam.
Symptoms You Should Pay Attention To
A subconjunctival hemorrhage often comes without warning and, in many cases, without any discomfort. Still, symptoms beyond the red patch can tell you whether it’s just a cosmetic issue or a signal to get medical help. Below are the most common signs, explained with details on duration, intensity, and seriousness.
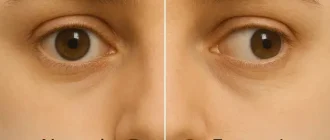
Painless Red Patch
Most people simply see a red spot on the sclera without feeling anything else. This is the classic presentation and is almost always harmless. Seriousness: Minimal; monitor at home.
Scratchiness or Mild Irritation
A light scratchy or gritty feeling may occur because the conjunctiva is slightly raised where blood collects. It usually feels like a speck of dust and disappears in a day or two with lubricating drops. Seriousness: Mild; comfort treatment only.
Eye Pain
Pain is the real differentiator. If discomfort is fleeting (for example, a dull ache on waking that fades in minutes), it is less concerning. But persistent, throbbing, or sharp pain lasting hours suggests something beyond a surface bleed, such as increased pressure or corneal involvement. Seriousness: Moderate to severe; requires prompt exam.
Sensitivity to Light (Photophobia)
Occasional light sensitivity can happen with dry eyes or fatigue, but sudden photophobia that lingers throughout the day may indicate inflammation inside the eye. Patients often describe needing sunglasses indoors. Seriousness: Significant; medical evaluation needed.
Blurred or Reduced Vision
Vision changes are never normal in a simple subconjunctival hemorrhage. If you notice blurring, shadowing, or decreased acuity that lasts beyond a few minutes, it could point to glaucoma, hyphema, or retinal problems ⧉. Seriousness: High; urgent attention required.
Recurrent Hemorrhages
One isolated red spot is usually nothing. But if hemorrhages occur several times a year, it raises suspicion for uncontrolled hypertension, diabetes, or medication side effects. Think of it as a smoke alarm going off repeatedly — the underlying fire must be checked. Seriousness: High; full medical workup advised.
Effectiveness of Symptom Relief Methods
Artificial tears — 70%
These drops work best because they act directly on the irritated surface, giving fast and reliable comfort.
Cold compresses — 50%
Cooling reduces mild swelling and eases irritation, but it does not address the vessel itself, so relief is partial.
Rest and sleep — 40%
General rest supports overall recovery and is always helpful, but by itself it only modestly improves eye comfort.
Pain relievers (Tylenol®) — 60%
They reduce headache or pressure discomfort, but since they don’t act on the eye surface, effect is supportive, not curative.
Source: eyexan.com
Editorial note: Reyus Mammadli reminds patients that short-lived discomfort is rarely dangerous, but ongoing pain, prolonged light sensitivity, or repeated bleeds are red flags not to ignore.
Real-Life Cases From the U.S.
Stories from everyday people help bring clarity to what otherwise feels like a confusing red patch. These snapshots show how broken blood vessels in the eye can appear in very different circumstances, and how patients responded.
Case 1: Houston, TX — Male, 42
One morning after an intense gym session that included heavy deadlifts, he glanced in the locker room mirror and noticed what looked like a red paint splash in his right eye. At first, he thought he had scratched himself with chalk-dusted fingers.
There was no pain or change in vision, but the size of the red patch grew during the day. Concerned, he called his optometrist, who examined him the same afternoon with a slit lamp. The diagnosis was a simple subconjunctival hemorrhage.
He was reassured, told to use preservative-free tears (like Systane Ultra) for comfort, and the spot faded within about 12 days. He later commented that knowing it was “just a bruise in the eye” made him much less anxious the next time it happened.
Case 2: Chicago, IL — Female, 66
This patient began noticing small red patches every few months, usually on waking in the morning. She would go to bed with clear eyes and wake up with what looked like a bloodshot stain on one side. Over time, the hemorrhages became more frequent, and she finally scheduled an exam.
At her appointment, her blood pressure measured 168/96 mmHg. The ophthalmologist immediately referred her to her primary care physician, who adjusted her hypertension medications. Within three months, not only did her general health improve, but the eye hemorrhages stopped completely.
Her case illustrates how a “harmless” red spot can be the first warning sign of an underlying cardiovascular problem.
Case 3: Boston, MA — Female, 25 (Graduate Student)
During a winter flu season, she developed a severe cough that lingered for a week. On the fourth day, she noticed both eyes had turned bright red after a particularly intense coughing fit during the night. Alarmed, she visited the student health center the next morning.
The clinician performed a slit-lamp exam and ordered basic blood tests to rule out clotting disorders. Results were normal, and she was advised to control the cough with prescribed medication and stay hydrated.
Over the next two weeks, the redness faded completely. She later remarked that the symmetrical appearance in both eyes had scared her the most, but understanding the link between pressure spikes from coughing and eye vessels breaking helped her manage her anxiety.
How Doctors Diagnose a Broken Blood Vessel in the Eye
Diagnosis usually starts with a simple exam using a slit lamp — a microscope with a bright light that allows an ophthalmologist to inspect the surface of the eye. If there’s no pain, vision loss, or history of trauma, further testing may not be needed.
When the cause is unclear or the condition keeps coming back, additional tests may be ordered:
- Intraocular pressure check (tonometry): Screens for glaucoma.
- Optical Coherence Tomography (OCT): High-resolution imaging of the retina and optic nerve. Accuracy: 9.5/10. Cost: $150–$300 ⧉.
- Fluorescein angiography: Uses dye to evaluate retinal blood vessels. Accuracy: 9/10. Cost: $200–$500.
- Blood tests (CBC, INR): Check for clotting disorders or medication effects.
| Test | Purpose | Accuracy (1–10) | Average U.S. Cost |
|---|---|---|---|
| Slit-lamp exam | Surface bleeding, corneal health | 9 | $100–$200 |
| Tonometry | Eye pressure (glaucoma screen) | 8 | $20–$60 |
| OCT | Retina, optic nerve imaging | 9.5 | $150–$300 |
| Fluorescein angiography | Abnormal retinal vessels | 9 | $200–$500 |
| CBC/INR | Blood counts, clotting status | 7 | $30–$80 |
Below is what these tests actually involve in everyday terms:
- Slit-lamp exam: The doctor uses a special microscope with a bright light, sitting across from you much like an eye‑test machine. No pain, no drops needed. Think of it as a magnifying glass on steroids to look at the surface of the eye.
- Tonometry (eye pressure test): A quick puff of air or a gentle probe after numbing drops. It feels odd but not painful. The machine is checking how “firm” the eye is, like squeezing a ball to see if it’s too tight.
- Optical Coherence Tomography (OCT): You place your chin on a rest, look at a small target light, and the scanner captures images in seconds. It’s as painless as taking a photo, but instead of a selfie, the camera takes cross‑section pictures of the back of your eye.
- Fluorescein angiography: First, a yellow dye is injected into your arm vein. Within seconds it travels to the eyes, and special cameras take pictures of blood flow in the retina. It’s safe, though your skin and urine may look a bit yellow for a day. The process is similar to turning on a highlighter inside your bloodstream so doctors can trace vessel leaks.
- CBC/INR (blood tests): A small blood sample is drawn from your arm, usually in the morning. Results are often ready the same day or within 24 hours. These tests check your blood’s clotting ability and general health markers.
Treatment Options for Subconjunctival Hemorrhage
A subconjunctival hemorrhage is often self-limiting, meaning the eye heals on its own. Still, patients often want to know what they can do to feel more comfortable, how to recognize when something stronger is needed, and what costs to expect. Here’s what treatment looks like in practice.
When No Treatment Is Needed
In uncomplicated cases, the body reabsorbs the blood naturally within 1–3 weeks. There is no direct way to “speed it up.” The spot gradually fades, much like a bruise on the skin. Effectiveness: 100% for simple cases, as nature does the work. Cost: none. Purpose: observation only.
Over-the-Counter Relief
Artificial tears (lubricating drops): Brands like Systane Ultra or Refresh Tears are sold in any U.S. pharmacy for $10–$20 per bottle. They soothe dryness or scratchiness by adding moisture to the surface. Relief usually appears within minutes. If symptoms persist beyond 2–3 days despite frequent use (4–6 times per day), switching brands or preservative-free formulations may help. Effectiveness: Symptom relief only, does not heal the bleed itself.
Acetaminophen (Tylenol®): For mild headache or discomfort, a typical dose costs less than $0.50. It works within 30–60 minutes. Importantly, NSAIDs like ibuprofen can thin blood slightly and are less preferred in this setting. Effectiveness: Reduces pain, does not change eye healing.
Medical Interventions for Complicated Cases
Hyphema treatment: If blood pools inside the front chamber of the eye, urgent management is needed. Doctors may prescribe steroid drops to reduce inflammation, pressure-lowering drops, or recommend surgical drainage if pressure rises dangerously. These procedures may cost $200–$800 for initial emergency care, with higher costs if surgery is required. Effectiveness: High, but depends on timely intervention. Purpose: Prevents glaucoma and vision loss.
Post-surgery hemorrhage care: After LASIK or cataract surgery, surface hemorrhages are common. Surgeons typically advise observation and lubricating drops, but will examine the eye to rule out infection or pressure changes. Follow-up visits average $100–$200 each. Effectiveness: High for ruling out complications. Purpose: Monitoring more than active treatment.
How to Judge if Treatment Works
- If using lubricating drops, comfort should improve within 1–2 days. If irritation remains or worsens, try a preservative-free brand or consult a doctor.
- If pain, vision changes, or new symptoms appear at any time, over-the-counter care is not enough — professional evaluation is required.
- Hyphema or trauma-related bleeding always demands urgent treatment, regardless of comfort level.
Editorial note: Reyus Mammadli advises patients to see artificial tears as “a band-aid for comfort, not a cure.” The red spot will fade on its own; the main role of treatment is easing irritation and ruling out serious complications.
Average Healing Time for Eye Hemorrhage
Healthy patients without risk factors — 7–10 days
Quick healing happens because vessels are strong and recover fast. Staying hydrated and resting eyes speeds recovery.
Patients with hypertension — 10–14 days
High blood pressure slows healing by stressing fragile vessels. Controlling pressure with diet and medication improves recovery.
Patients on blood thinners — 14–20 days
Blood-thinning drugs make clots form slowly, extending healing. Regular checkups and careful monitoring shorten the timeline safely.
Post-surgery patients — up to 21 days
After LASIK or cataract surgery, healing is slower due to tissue stress. Following surgeon’s advice and avoiding strain ensures safe recovery.
Source: eyexan.com
Prevention: How to Protect Your Eyes From Broken Vessels
Broken blood vessels in your eye are not always avoidable, but several everyday habits can lower the risk dramatically. Here are the most practical ways to prevent them, with notes on effectiveness and who benefits most.
- Wear protective eyewear: Safety glasses rated by ANSI are inexpensive ($10–$30) and highly effective in shielding eyes from flying particles during sports, woodworking, or yard work. Best for anyone doing physical or outdoor tasks where debris is common.
- Manage high blood pressure: Keeping systolic/diastolic numbers in the normal range reduces repeat hemorrhages by lowering stress on fragile vessels. This is especially crucial for adults over 40 and those with a family history of hypertension. Lifestyle measures (diet, exercise, weight control) plus medications if prescribed make this highly effective.
- Avoid rubbing your eyes: Rubbing can create direct trauma, especially if a fingernail or small particle is involved. Teaching children this habit early and reminding contact lens wearers is simple and effective prevention.
- Review medications and supplements: Talk with your doctor if you take aspirin, warfarin, clopidogrel, or high-dose supplements like vitamin E or ginkgo ⧉. Adjusting dosage or timing may prevent recurrences. Particularly relevant for older adults and those on long-term heart medications.
- Post-surgery care: After LASIK or cataract surgery, avoid straining, bending, or heavy lifting in the first 1–2 weeks. Following the surgeon’s guidelines is highly effective at preventing pressure spikes and bleeding.
Reyus Mammadli highlights that prevention is “80% habit.” In other words, protecting your eyes is less about expensive treatments and more about smart everyday choices: keep your blood pressure checked, shield your eyes when they’re at risk, and avoid unnecessary strain.
Risks and Complications You Shouldn’t Ignore
A subconjunctival hemorrhage is usually harmless, but there are circumstances where it signals a deeper issue. Each complication below is explained not just in medical terms, but also in everyday language so you understand why it matters.
- Hyphema: This means blood collects inside the front chamber of the eye. Beyond the redness, it can raise eye pressure and trigger glaucoma, a disease that damages the optic nerve and can cause permanent vision loss or even blindness if untreated ⧉. Why it matters: What seems like a surface problem can actually be sight-threatening and may require surgery if not addressed quickly.
- Stroke risk: Repeated hemorrhages in older adults sometimes point to underlying vascular disease. While a single red eye is not a stroke, frequent events can act like a warning light on your car dashboard, telling you to check the engine. Why it matters: Vascular problems increase the chance of heart attack and stroke, conditions that can be life-altering or life-threatening ⧉.
- Uncontrolled hypertension or diabetes: These chronic conditions weaken blood vessels over time. In the eyes, they may first appear as tiny bleeds, but elsewhere in the body they raise the risk of kidney failure, heart disease, and other complications. Why it matters: A red patch may be the earliest visible clue that long-term diseases are silently causing damage.
In short, while most red spots fade without consequence, ignoring repeated or complicated cases could cost much more than peace of mind — it could cost your vision or overall health.
Questions to Ask Your Doctor
When you see your eye doctor, it helps to go in prepared. These questions not only guide the conversation but also show the doctor that you understand the importance of the issue. Here’s how each question can help you — and what to do with the answer.
- How severe is my hemorrhage and is it purely superficial?
Asking this clarifies whether it’s just a surface bruise or something deeper. The answer will guide whether you simply wait it out or if further tests and follow-ups are needed. - How long will it take to clear?
Knowing the typical timeline (days vs. weeks) helps set realistic expectations. If the redness lasts longer than what your doctor says, you’ll know it’s time to schedule a recheck. - Should I be checked for high blood pressure or clotting disorders?
This question links eye health to overall health. A “yes” means you should follow up with your primary care doctor for blood pressure monitoring or lab tests, potentially preventing serious cardiovascular events. - What treatment options are appropriate for me?
Different patients need different approaches — artificial tears, pressure-lowering drops, or just observation. The doctor’s answer helps you understand whether your plan is comfort-based or if it addresses a medical problem. - Could this affect my vision long-term?
This separates cosmetic concerns from sight-threatening ones. If the doctor signals a risk to vision, it’s a red flag to take treatment and follow-up seriously. - Do I need further tests like OCT or fluorescein angiography?
This ensures you don’t miss hidden retinal or vascular problems. If tests are recommended, you’ll know they are not optional extras but tools to protect your sight. - If this happens again, when should I call versus monitor at home?
The answer provides a clear action plan: when to wait calmly and when to seek urgent help. It helps you avoid unnecessary anxiety while still protecting your eyes.
By asking with purpose and understanding the meaning behind each answer, you empower yourself to make informed decisions about both your eye health and your general well-being.
Editorial Advice
According to medical consultant Reyus Mammadli, one isolated red patch is usually harmless. “But if you’re older, on blood thinners, or dealing with high blood pressure, don’t just ignore it,” he says. “Those cases require a closer look.”
Tips from the editorial team:
- Don’t panic if you notice a bright red spot — keep track of when it appeared and how it changes.
- If it lasts beyond three weeks, book an exam.
- Use preservative-free tears if you apply drops more than four times daily.
- Protect your eyes with safety glasses during risky activities.
With smart habits and awareness, you can handle a broken blood vessel in the eye calmly and protect your long-term vision.