The potentially sight-robbing vascular irregularity referred to as the carotid-cavernous sinus fistula (CCF) can masquerade as conjunctivitis or other typical ocular conditions, which decreases the opportunity for a quick medical diagnosis. However, treatment success rates for these fistulas now approach 100 percent when the repair work is carried out early by knowledgeable specialists. Contemporary endoscopic methods have likewise made treatment of these fistulas far less dangerous.
“Mortality from the treatments is incredibly unusual, and the morbidity is rather low — usually nothing more than double vision or some pain that disappears within a few days to a few weeks.
Prompt diagnosis, however, remains an obstacle. The medical diagnosis is typically missed out on, leading to months of unsuitable therapy and, in some patients, vision loss due to treatment hold-up.
Two Types of Arterial Diversion
CCFs are categorized as direct or dural.
Direct CCFs involve a tear or hole in a branch artery arising from the internal carotid artery within the cavernous sinus. These fistulas usually result from some injury, like an automobile mishap or mugging. However, some are iatrogenic, happening during a neurosurgical or interventional neuroradiological procedure. Moreover, others arise from a spontaneous rupture of a carotid artery aneurysm in the cavernous sinus.
Dural arteriovenous shunts are irregular communications between the cavernous sinus and one or more meningeal branches of the internal carotid artery, external carotid artery or both. Shunts including both arterial distributions are the most common. The pathogenesis of dural fistulas is uncertain; however, it appears that they stem from small arteriovenous shunts in the dura that are normal variations. For some factor — potentially the impacts of an angiogenesis element — the shunts start to multiply and become unusual. They are typically associated with occlusion in the nearby draining venous dural sinuses, such as the spacious sinus. All of a sudden there is little-arterialized blood flow into the venous system and a compromised egress of normal blood from the venous system because of thrombosis. The result is an asymptomatic arteriovenous shunt. Risk factors for the advancement of a dural CCF include systemic high blood pressure, atherosclerotic vascular disease, pregnancy, Ehlers-Danlos syndrome and small injury.
Subtle Signs and Symptoms of Carotid-Cavernous Fistulas

The medical presentation of a CCF is influenced by the type and size of the fistula along with its area, blood circulation rate, and drainage route. Some evidence recommends that lots of dural fistulas drain pipes posteriorly first– into the inferior petrosal sinus, basilar venous plexus or both– and after that anteriorly as the primary pathway becomes blocked. Posterior drain produces typically no ocular symptoms, although some patients may experience a cranial neuropathy, such as facial paresis or ocular motor nerve paresis. Ocular signs and symptoms usually develop as the drain moves to an anterior path through the remarkable and inferior ophthalmic veins. Since of their lower flow rate, dural CCFs usually produce less extreme symptoms than those from a direct CCF. Objective and subjective bruits likewise are less typical with dural fistulas.
Easy to misinterpret. Dural CCFs could have a subtle discussion, including a slightly red eye with little or no proptosis, elevation in intraocular pressure, moderate discomfort, secondary glaucoma, venous congestion to the retina and some ophthalmoparesis with double vision.
These patients are typically misdiagnosed as having thyroid eye disease or conjunctivitis or blepharitis. However several dead giveaways can indicate the diagnosis. Patients with an arteriovenous shunt or fistula usually have little, tortuous corkscrew-type capillary in the conjunctiva that comes near the limbus and appears different from those seen with the other ocular conditions. In contrast to generalized conjunctivitis, these vessels are localized to specific areas, such as the interpalpebral conjunctiva. IOP is elevated on the involved side, and standard applanation tonometry reveals a bigger ocular pulse amplitude in that eye compared to the noninvolved eye. Ophthalmoscopic findings can be healthy, or they might expose a minor dilation of the retinal veins.
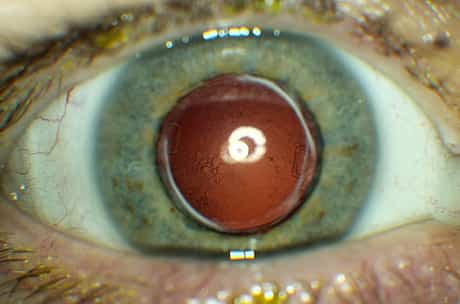
When worse becomes worse. Advanced dural fistulas, especially those with substantial orbital or cavernous sinus venous occlusion, might trigger periorbital or retrobulbar discomfort and possibly facial pain. Increasing episcleral venous pressure can increase intraocular pressure. The elevated venous pressure in orbit, blockage in the iris and choroid and displacement of the iris-lens diaphragm might result in angle-closure glaucoma. Ophthalmoscopic findings might consist of intraretinal hemorrhages; retinal detachments; vitreous hemorrhages; choroidal folds, effusions, and detachments; or swelling of the disc.
Postponed medical diagnosis puts vision at risk. Failure to recognize the different characteristics of the red eye that arises from a dural fistula compared to those seen with an inflammatory process or glaucoma can send patients on a discouraging odyssey from one ophthalmologist to another.
Some ophthalmologists will take a look at the red eye quickly and offer an antibiotic or steroid drop. They might not even inspect the patient’s pressure out of an issue that it is an infectious procedure. When the client comes back with elevated pressure, the eye doctor thinks it might rise because of the steroid drops — so eye doctors are missing the process. People who pertain to see us are intensified since they have been from medical professional to medical professional for month upon month up until someone finally puts everything together. He added that patients with an irregular red eye might be asked whether they hear a pulsatile bruit.
About 20 to 30 percent of all dural fistulas lead to vision loss, typically due to unrestrained glaucoma, ischemic optic neuropathy or chorioretinal dysfunction.
How to get the proper medical diagnosis. A catheter angiogram is the best diagnostic test for CCFs. However, ophthalmologists who presume a fistula can purchase one or more noninvasive imaging studies to support their suspicions. These options include computed tomography, angiography, contrast-enhanced magnetic resonance imaging that concentrates on the spacious sinus and MR angiography that does not “cut off” the dural arteries.
Ophthalmologists can order an MRI with contrast, explaining to the neuroradiologist that they are searching for an arteriovenous shunt to the spacious sinus. The more info they provide the neuroradiologist, the much better the information they will receive in return. The ophthalmologist also must ask the neuroradiologist to make certain there is no precarious or irregular venous drain from the brain.
Endovascular Treatment
Dr. Miller said that patients with moderate ocular symptoms could be observed to identify whether the fistula will close spontaneously, as do about 20 to 50 percent. During this observation period, patients’ visual function, IOP and ophthalmoscopic appearance ought to be kept an eye on frequently.
Consistent diplopia can be managed with prism treatment or occlusion of one eye, and proptosis-related keratopathy can be eased with ocular lubrication.
For significantly raised IOP topical agents be tried for a couple of weeks. If IOP stays significantly elevated, closure of the fistula is the best treatment. Intraocular surgery to control secondary glaucoma or unrelated cataract carries a high threat since of the orbital venous hypertension.
Close hole, keep the artery open. Fortunately, treatment security and success have increased drastically over the years. Previously, in many cases, absolutely nothing was done since you would need to close the whole internal carotid artery or the external carotid artery, or both, and there was a risk of stroke and neurologic dysfunction. Today individuals can be dealt with reasonably noninvasively with endovascular techniques in which compounds such as glue or platinum coils are put in the fistula, with conservation of the major artery.
Platinum is the new gold. The successful closure rate with detachable platinum coils ranges from 90 to100 percent. These coils stay the preferred material at the University of California, Los Angeles, where they were established. “Work is constantly being done on some of the newer agents – for example, some of the foams– however for fistulas in the spacious sinus, I believe the choice here is still coils.
Calling professional collaborators. Some dural fistulas can be treated by an interventional neuroradiologist alone, whereas others require a group technique. Having an orbital professional or neuro-ophthalmologist involved is often useful. Sometimes there is the need to access the vein through the orbit. Also, treatment decision-making is sometimes complicated and depends upon the status of the optic nerve and the degree of vascular compromise. Having an expert from the ophthalmology side take part in the decision-making, and the follow-up of the orbit is important for the patient.
This is an experienced strategy that requires an eye doctor who has training and an understanding of how to do this.