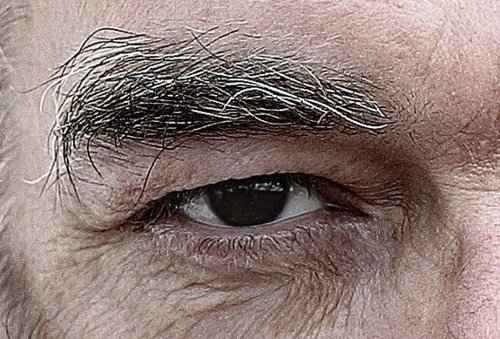
When it comes to sight-saving medical procedures, few are as transformative as corneal transplantation. It is a complex, highly specialized surgery, where a damaged or diseased cornea is replaced with a healthy donor cornea. Corneal transplants are essential for restoring vision in individuals whose corneas have been compromised due to injury, disease, or infection. Today, let’s delve into the intricacies of corneal transplantation surgery, its recent advancements, and the reality behind patient outcomes.
The Evolution of Corneal Transplants: From Full to Selective Transplants
Historically, the term “corneal transplant” would evoke images of full-thickness corneal replacement, a technique known as Penetrating Keratoplasty (PK). However, medical science has come a long way, and now we see selective corneal transplantation techniques on the rise. Endothelial Keratoplasty (EK) and Deep Anterior Lamellar Keratoplasty (DALK) are leading the way as newer, more refined methods of treating specific layers of the cornea.
Types of Corneal Transplantation Surgery
| Type of Surgery | Description | Success Rate |
|---|---|---|
| Penetrating Keratoplasty (PK) | Full-thickness replacement of the cornea with donor tissue. | 70-85% in 5 years |
| Endothelial Keratoplasty (EK) | Selective replacement of the inner corneal layer (endothelium). | 85-95% in 5 years |
| Deep Anterior Lamellar Keratoplasty (DALK) | Replacement of the outer corneal layers, preserving the endothelium. | 80-90% in 5 years |
With the increased precision of these modern methods, success rates have improved, and the risk of complications such as rejection has decreased significantly. The selective techniques help preserve as much of the patient’s original corneal structure as possible, reducing trauma and recovery time.
Corneal Blindness: How Prevalent Is It?
The World Health Organization (WHO) estimates that corneal diseases are the fourth leading cause of blindness globally. Approximately 12.7 million people are currently awaiting a corneal transplant. Unfortunately, there is a significant gap between donor supply and demand—it’s estimated that only one in 70 patients who require a corneal transplant receives one.
This gap is more pronounced in developing countries, where access to corneal tissue is scarce, and infrastructure for donation and transplantation is underdeveloped. In contrast, developed nations have benefited from enhanced corneal donation awareness campaigns and well-organized eye banks, bridging the gap more effectively.
Why Do Patients Need Corneal Transplants?
The reasons for corneal transplants are varied, but the most common include:
- Keratoconus: A progressive thinning of the cornea that causes it to bulge into a cone shape, distorting vision.
- Fuchs’ Dystrophy: A condition where the cells in the inner layer of the cornea (endothelium) gradually deteriorate, leading to corneal swelling and visual impairment.
- Corneal Scarring: Resulting from infections (such as herpes simplex) or trauma, which can significantly impact vision.
Real-World Example: Keratoconus and DALK
One notable advancement in treating keratoconus is the use of Deep Anterior Lamellar Keratoplasty (DALK). In this procedure, only the damaged outer layers of the cornea are replaced, while the healthy endothelium is retained. This reduces the risk of graft rejection—a common complication in full-thickness corneal transplants.
Dr. Jonathan Ruiz, a corneal specialist, shares, “DALK is a game-changer for keratoconus patients. By preserving the patient’s endothelium, we significantly lower the likelihood of rejection, which has been one of the biggest challenges in corneal transplantation.”
Success Rates and Complications: The Truth Behind the Numbers
While the success rates for corneal transplantation are generally high, they are not without risks. Rejection remains a primary concern, particularly for full-thickness transplants. Studies show that about 20-30% of PK patients experience rejection episodes within the first five years.
Selective transplants, such as EK and DALK, have shifted the landscape positively, with rejection rates now below 10% in many cases. Here’s a look at some of the common complications and their occurrence rates:
| Complication | Occurrence Rate in PK (%) | Occurrence Rate in EK/DALK (%) |
|---|---|---|
| Graft Rejection | 20-30% | <10% |
| Infection | 1-2% | <1% |
| Astigmatism | 15-25% | 5-10% |
Astigmatism is another frequent issue after corneal transplantation, particularly with PK, as the entire cornea is replaced. The irregular healing of the tissue can lead to a distorted corneal surface, affecting vision quality. EK and DALK, on the other hand, tend to result in much lower levels of astigmatism due to their more targeted approach.
Emerging Trends and Technological Innovations
The field of corneal transplantation has been transformed by advancements in tissue engineering and regenerative medicine. Researchers are exploring alternatives such as biosynthetic corneas to address the donor tissue shortage. A recent study published in Nature Biotechnology revealed that biosynthetic implants could restore vision in 76% of participants with corneal blindness—a promising step toward reducing global reliance on donor tissue.
Another exciting trend is the use of Descemet Membrane Endothelial Keratoplasty (DMEK), an even more selective form of EK that replaces only the Descemet membrane and endothelium. This technique offers faster recovery times and a more stable visual outcome, with success rates as high as 95%.
Patient Perspective: The Emotional Journey
Beyond the numbers, corneal transplantation is a profoundly personal journey for patients. Martha, a 58-year-old woman who underwent EK for Fuchs’ dystrophy, describes her experience: “I was losing my ability to see the faces of my grandchildren clearly. The surgery gave me back something I thought I’d lost forever. Recovery was challenging, but the outcome was worth every moment.”
Our Editorial Advice for Patients Considering Corneal Transplantation
If you or a loved one is considering corneal transplantation, it is crucial to weigh the risks and benefits based on your specific condition. Discuss the different types of corneal transplants with your ophthalmologist and understand which option best suits your needs. The advancements in selective transplants, such as EK and DALK, offer promising outcomes with reduced risks, especially for conditions like keratoconus or Fuchs’ dystrophy.
Our team recommends prioritizing centers with experience in the latest techniques and a robust post-operative care program. Remember, while the road to recovery can be bumpy, the potential to regain clear vision makes it a journey worth taking. As Dr. Ruiz puts it, “The success of corneal transplantation is not just in the surgery—it’s in the follow-up, the care, and the patient’s determination to heal.”
Corneal transplantation is a beacon of hope for millions suffering from impaired vision. Armed with the right information and a dedicated medical team, you can reclaim the gift of sight and embrace life with a clearer view.