A cornea transplant replaces diseased or scarred corneal tissue with healthy tissue from an organ donor. There are two main types of cornea transplants: conventional, full thickness cornea transplant (also known as penetrating keratoplasty, or PK) and back layer cornea transplant (likewise called endothelial keratoplasty, or EK).
Corneal Transplantation Surgery Overview
A graft replaces main corneal tissue, harmed due to disease or eye injury, with healthy corneal tissue contributed from a regional eye bank. An unhealthy cornea affects your vision by scattering or distorting light and triggering glare and blurred vision. A cornea transplant may be essential to restore your practical vision.
Corneal eye disease is the fourth most common reason for blindness (after cataracts, glaucoma and age-related macular degeneration) and impacts more than 10 million people worldwide.
More than 47,000 cornea transplants will be carried out in the United States in 2013, according to an evaluation by the Eye Bank Association of America. Given that 1961, more than one million people have actually had their sight restored with a cornea transplant.
When Do You Need a Cornea Transplant?
A healthy, clear cornea is important for excellent vision. If your cornea is harmed due to eye disease or eye injury, it can become swollen, scarred or severely misshapen and distort your vision.
Normally growing eyelashes versus eyelashes that are growing towards the eye, which is called trichiasis.
A corneal transplant may be needed in cases of conditions such as trichiasis, where eyelashes turn inward and rub against the surface area of the eye, triggering scarring and vision loss.
A cornea transplant might be required if glasses or contact lenses can’t restore your functional vision, or if painful swelling cannot be alleviated by medications or unique contact lenses.
Particular conditions can affect the clearness of your cornea and put you at higher risk of corneal failure. These consist of:
- Scarring from infections, such as eye herpes or fungal keratitis.
- Scarring from trichiasis, when eyelashes grow inwardly, toward the eye, and rub against the cornea.
- Genetic conditions such as Fuchs’ dystrophy.
- Eye illness such as innovative keratoconus.
- Thinning of the cornea and irregular corneal shape (such as with keratoconus).
- Rare complications from LASIK surgery.
- Chemical burns of the cornea or damage from an eye injury.
- Extreme swelling (edema) of the cornea.
- Graft rejection following a previous corneal transplant.
- Corneal failure due to cataract surgery complications.
Are You a Cornea Transplant Candidate?
A cornea transplant is performed to improve the function of the cornea and enhance vision. If pain is triggered by a considerably diseased or damaged cornea, a cornea transplant may ease that symptom.
BEST CANDIDATES:
harmed cornea due to disease or eye injury, distorted vision.
- Procedure time: one to two hours.
- Normal results: significant improvement in visual function.
- Recovery time: numerous weeks to a year.
With these factors in mind, you also ought to think about several crucial questions prior to you decide to go through a corneal transplant:.
- Does your practical vision impede your job efficiency or your capability to carry out everyday activities?
- Can your vision be corrected with special contact lenses or other less invasive measures?
- How will the cost of cornea transplant surgery affect your financial scenario if your vision insurance does not cover everything from pre-screening to post-operative assessments?
- Are you able to take enough time off from work or school (up to 6 months to a year sometimes) to recover properly?
All of these questions, in conjunction with a comprehensive screening and consultation with your eye doctor, should be thoroughly thought about prior to you make the final decision to have a corneal transplant.
Prior to Corneal Transplantation Surgery
As soon as you and your eye doctor choose a cornea transplant is the best alternative for you, your name is put on a list at a regional eye bank. You may have to wait a few days to weeks for suitable tissue from a donor eye to become readily available for a corneal transplant.
Prior to a donor cornea is launched for use in transplant surgery, it is looked for clearness and screened for the presence of any illness such as hepatitis and AIDS, in accordance with the Eye Bank Association of America’s stringent medical standards and FDA regulations.
Just corneas that satisfy these strict guidelines are used in corneal transplant surgery to guarantee the health and safety of the graft recipient.
BenefitsPalSave 10-30% off your eye test using the BenefitsPal ™ cardFind an eye doctor with the Think About Your Eyes Doctor LocatorWhat is more important than your vision? Find local optometrist to obtain an eye examination.
During the Cornea Transplant
Your eye surgeon will first administer either local or basic anesthesia, depending upon your health, age, eye injury or disease, and whether you choose to be asleep during the procedure.
If local anesthesia is used, an injection is made into the skin around your eye to unwind the muscles that control blinking and eye movements, and eye drops are used to numb your eye. You will be awake during the procedure and many people don’t report any pain.
After the anesthesia has worked, an instrument called a cover speculum is used to keep your eyelids open. Your cosmetic surgeon then measures the affected corneal area to identify the size of the donor tissue needed.
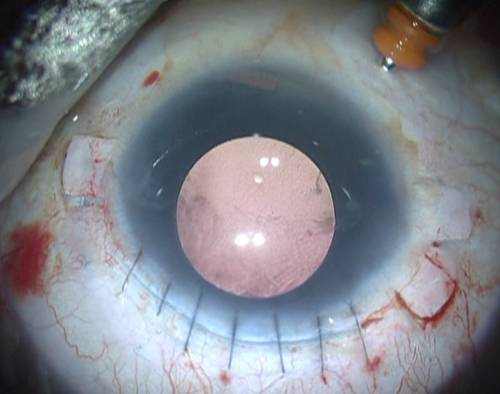
Standard corneal transplant surgery. During standard corneal transplant surgery, or penetrating keratoplasty (PK), a circular button-shaped, full-thickness section of tissue is gotten rid of from the diseased or injured cornea using either a surgical cutting instrument called a trephine or a femtosecond laser.
A matching “button” from the donor tissue is then placed and sutured into place. The stitches (stitches) remain in place usually for a year or more after surgery.
Lastly, a plastic guard is placed over your eye to safeguard it during recovery.
Permeating keratoplasty surgery normally takes one to two hours and most treatments are performed on an outpatient basis, implying you can go home a brief while after the surgery (though you will need someone to own you home).
Donor cornea sutured in place of an eliminated cornea.
Who Can Be a Corneal Tissue Donor?
How old is too old to donate eye tissue for a corneal transplant? A decade earlier, it was common for cosmetic surgeons to reject corneas from individuals over 65 years old. But the Cornea Donor Study has concluded that corneas from individuals aged 34-71 are most likely to stay healthy for a lot of receivers after 10 years, with a success rate of 75 percent.
In the United States, about three-quarters of corneas come from this age range, with one-third from people aged 61-70.
Endothelial keratoplasty. In the previous years, a newer variation of corneal transplant surgery called endothelial keratoplasty (EK) has been presented for certain corneal conditions.
Endothelial keratoplasty selectively changes just the inner layer of the cornea (endothelium) and leaves the overlying healthy corneal tissue intact. The endothelium controls the fluid balance in the cornea, and if it becomes broken or infected, this can cause significant corneal swelling and loss of vision.
In EK, the cosmetic surgeon makes a tiny incision and puts a thin disc of donor tissue consisting of a healthy endothelial cell layer on the back surface area of your cornea. An air bubble is used to place the new endothelial layer into place. The little incision is self-sealing and usually no stitches are required.
The most typical type of EK procedure is called Descemet’s Stripping Endothelial Keratoplasty, or DSEK. The American Academy of Ophthalmology in 2009 backed DSEK as superior to the standard full-thickness corneal transplant procedure (penetrating keratoplasty) for much better vision outcomes and stability, along with less risk factors.
Endothelial keratoplasty has several benefits over full-thickness penetrating keratoplasty. These consist of: faster recovery of vision; less operating time; very little removal of corneal tissue (and for that reason less effect on the structural stability of the eye and less susceptibility to injury); no associated suture complications; and minimized risk of astigmatism after surgery.
Within a fairly brief amount of time, the EK corneal graft procedure has ended up being the favored strategy for patients with Fuchs’ dystrophy and other endothelial conditions of the cornea. However, traditional full-thickness PK is still the most proper choice when the majority of your cornea is diseased or scarred.
Recovering From a Cornea Transplant
Total cornea transplant recovery time can be as much as a year or longer. At first, your vision will be blurred for the first few months– and in many cases might be even worse than it was before– while your eye gets used to its brand-new cornea.

As your vision enhances, you slowly will be able to go back to your normal everyday activities. For the first numerous weeks, heavy workout and lifting are prohibited. However, you ought to be able to return to work within a week after surgery, depending upon your job and how quickly your vision improves.
Steroid eye drops will be prescribed for a number of months to assist your body accept the brand-new corneal graft, along with other medications to help control infection, discomfort and swelling. You should keep your eye secured at all times by using a guard or a set of glasses so that absolutely nothing accidentally bumps or enters your eye.
If stitches were used in your surgery, they typically are removed 3 to 17 months post-surgery, depending upon the health of your eye and the rate of healing. Adjustments can be made to the sutures surrounding the brand-new corneal tissue to help lower the amount of astigmatism arising from an irregular eye surface.
Similar to any type of surgery, always follow the instructions of your eye cosmetic surgeon to help minimize corneal transplant complications and expedite healing.
Cornea Graft Rejection
Cornea transplants are carried out regularly and have a reasonable success rate. In truth, cornea grafts are the most effective of all tissue transplants.
Cornea transplant rejection can be reversed in 9 from 10 cases if detected early enough.
Like any other surgery, a cornea transplant includes particular risks. But, for most people, having their vision enhanced or brought back outweighs the prospective complications connected with cornea transplant surgery. It is a very personal decision for a patient to choose to go through cornea transplant surgery.
Complications of a corneal transplant can be considerable and can include cornea graft rejection, eye infection and issues connected with using stitches.
Rejection of the donor tissue is the most serious issue after a corneal transplant and takes place in 5 to 30 percent of patients. Transplant rejection is when your body’s immune system discovers the donor cornea as a foreign body and attacks and attempts to ruin it.
Research ** shows that having glaucoma and corneal swelling associated with previous cataract surgery can increase your chances of cornea graft rejection.
Acknowledging the primary warning signs of corneal transplant rejection is the first step to preventing graft failure. These can be kept in mind using the acronym RSVP:
- Redness.
- Extreme Sensitivity to light.
- Reduced Vision.
- Pain.
Rejection signs might happen as early as one month or as late as several years after surgery. Your eye doctor will prescribe medication that can assist reverse the rejection process. If discovered early, the graft will succeed 9 out of 10 times, according to the Cornea Research Foundation of America.
Must your graft stop working, corneal transplant surgery can be repeated. While repeat surgery usually has good outcomes, general rejection rates increase with the number of corneal transplants you have.
Vision After a Cornea Transplant
Your vision needs to gradually improve a couple of weeks after a corneal graft, but it might take anywhere from a couple of months as much as a year to have steady vision in the eye that gets the donor tissue.
After your cornea transplant has actually completely healed, it’s possible to go through LASIK eye surgery to enhance your vision (check out an average cost of LASIK procedure).
You will be entrusted to a degree of myopia (nearsightedness) and astigmatism, since the curve of the brand-new corneal tissue cannot match exactly the curve of your natural cornea.
Post-surgery refraction is rather unpredictable, and big quantities of astigmatism will still present an obstacle when fitting those patients with glasses later on.
Moderate refractive errors caused by corneal transplant surgery can be fixed with glasses; otherwise contact lenses are required.
Rigid gas permeable contact lenses, likewise known as RGP or GP lenses, and hybrid contact lenses typically are the most appropriate contacts for corneal transplant patients due to the irregularity of the cornea after transplant. However, soft contact lenses frequently are an alternative also.
Due to the fact that your vision will change during the first few months following your surgery, it is recommended to wait up until your eye doctor tells you your vision is stable before you fill an eyeglass prescription or are fitted for contact lenses.
After your eye has fully recovered and any stitches used have been gotten rid of, you may be qualified to undergo laser eye surgery such as LASIK or PRK to enhance your capability to see with or without glasses or contacts by reducing myopia and astigmatism.
Artificial Corneas and Biosynthetic Corneas
Human donor tissue is the chosen– and most effective– alternative for replacing an unhealthy or injured cornea. However, for patients who are at high risk of corneal transplant failure with a human donor (such as multiple failed human cornea transplants) and have no other options to enhance vision, synthetic cornea tissue might be used.
Synthetic corneas, also called “keratoprosthesis” or “K-pro”, are made from a biologically inert product and usually are reserved for patients who have: a severe autoimmune disease; chemical burns; limited or no access to human donor tissue; or have actually had numerous previous human donor transplant failures.
Another area of ongoing research is biosynthetic corneas. The outcomes from a recent early-phase scientific trial has actually revealed that a biosynthetic cornea made from a human gene that manages the natural production of collagen can restore and repair harmed eye tissue.
While the field of biosynthetic corneas is still in its infancy, with additional research this approach possibly could be a reliable alternative if human donor tissue is not suitable or available.