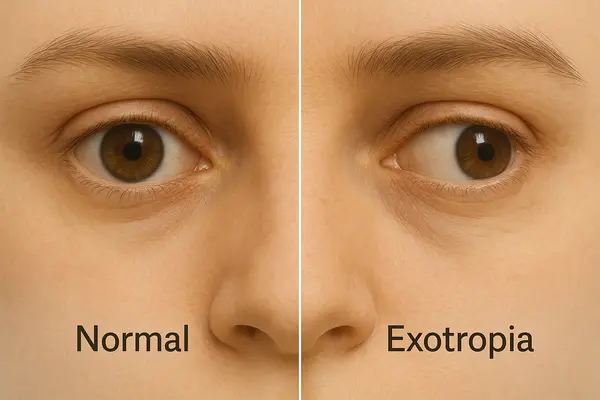
Exotropia, often referred to as “wall-eyes,” is a form of strabismus where one or both eyes turn outward, away from the nose. It can be constant or intermittent and is more visible when a person is tired, daydreaming, or focusing on distant objects. Unlike esotropia (crossed eyes), exotropia causes the eyes to diverge. This condition can affect both children and adults.
Types of Exotropia Diagnosed in Children (2023)
This chart illustrates the distribution of exotropia types diagnosed in children in 2023. Intermittent exotropia accounts for the majority of cases, while divergence excess and congenital types are less frequently observed.
Who’s at Risk?
Exotropia affects approximately 1% of the U.S. population, with higher rates in Asian and African-American communities. Genetics play a major role—if one parent has strabismus, the child has a 23% higher chance of developing it. Premature birth and low birth weight are also associated risk factors.
A 2021 study published in JAMA Ophthalmology analyzed over 4,000 pediatric eye exams and found that children with delayed visual development before age 2 had a 35% greater risk of developing some form of strabismus, including exotropia. Additionally, environmental and regional differences may play a role: children growing up in areas with limited access to pediatric eye care tend to be diagnosed later, sometimes after symptoms become more severe.
Interestingly, while exotropia can appear in adulthood, it is much more commonly diagnosed in childhood, with peak onset between ages 3 and 6. According to the American Association for Pediatric Ophthalmology and Strabismus (AAPOS), the female-to-male ratio is nearly equal, but girls are more likely to be brought for evaluation earlier due to greater parental concern over cosmetic appearance.
What Causes Exotropia?
Exotropia results from imbalances in the eye muscles or nerve signals that coordinate eye movement. But what does that really mean in everyday terms? Imagine your eye muscles are like the strings on a marionette. If one string pulls too tight or gets loose, the puppet (in this case, your eye) won’t move smoothly. That’s exotropia.
Exotropia vs. Esotropia Prevalence in Pediatric Strabismus Cases
| Type | Prevalence (%) |
|---|---|
| Exotropia | 38% |
| Esotropia | 62% |
This chart compares the prevalence of exotropia and esotropia in pediatric strabismus cases. Esotropia remains the more common type, representing 62% of diagnoses, while exotropia accounts for 38% of cases.
Here’s a closer look at the common causes and what they mean practically:
- Congenital muscle weakness: Some children are born with weaker muscles that control eye alignment. Think of it like a bicycle with one loose brake cable—the wheel doesn’t respond as evenly. If muscles around one eye are underdeveloped, the eye might drift outward instead of working in sync. This outward drift is characteristic of exotropia, often called wall eyes, especially when the deviation becomes noticeable during distance viewing.
- Neurological conditions (e.g., cerebral palsy, Down syndrome): These affect how the brain communicates with the muscles. If the control center (the brain) can’t properly send or receive messages to eye muscles, the coordination fails. It’s similar to giving someone directions with bad phone reception—they might not end up where you want them. In some patients, weakened neural control amplifies the outward turn seen in wall eyes.
- Trauma or eye surgery: Injuries or previous procedures can damage the delicate balance of muscle tension. For example, if you’ve ever tried to re-tie shoelaces after one has snapped, you know the balance feels off. The same happens with muscle healing—scar tissue or imbalance can pull one eye outward.
- Refractive errors, particularly myopia (nearsightedness): When the eyes constantly struggle to focus on distant objects, the brain might adjust by letting one eye drift outward to reduce the workload. It’s a bit like giving up trying to align a crooked picture frame—you stop correcting it, and it hangs off-center.
- Visual deprivation in early development: If a child doesn’t get enough stimulation (like from a cataract or untreated blurry vision), the brain may not learn to coordinate the eyes correctly. The eye without visual input essentially “checks out” and turns away.
Recognizing the Symptoms
Parents often notice children squinting or covering one eye to improve focus. Other symptoms include:
- Double vision: While many conditions can cause double vision, in exotropia it usually occurs when one eye starts to drift outward and both eyes stop working in coordination. The double images may improve when one eye is closed or when the person is resting.
- Eye fatigue: This is not just general tiredness, but a sensation of the eyes feeling strained after reading or screen time. In exotropia, fatigue tends to appear sooner and more intensely, especially when trying to focus on near objects.
- Difficulty reading: People with exotropia may lose their place frequently, skip lines, or avoid reading altogether. This is due to poor binocular coordination, which disrupts smooth eye tracking across a page.
- Poor depth perception: This is a strong indicator of exotropia. Activities that require precise judgment of distance—like catching a ball or pouring liquid—become difficult. If a person often stumbles or misjudges steps, this may be the reason.
- Eyes appearing to drift outward, especially during illness or stress: This classic sign of intermittent exotropia typically becomes noticeable when the person is fatigued, emotionally overwhelmed, or staring into the distance. It may not be present all the time but is more likely to emerge under these conditions.
Each of these symptoms may overlap with other eye conditions, but exotropia is uniquely characterized by outward eye deviation that becomes more visible during moments of low concentration or bright light exposure. If multiple symptoms appear together, especially with visible drifting, a clinical evaluation is essential.
Types of Exotropia
- Intermittent Exotropia: This is the most frequently diagnosed type and often appears when the patient is tired, sick, or focusing on something far away. It’s most noticeable during periods of inattention or fatigue. The eye may appear straight most of the time but will occasionally drift outward, especially in bright sunlight or when daydreaming. Patients may close one eye in bright light to avoid double vision.
- Constant Exotropia: In this form, the outward deviation is always present and more pronounced. The affected individual rarely achieves binocular fusion, meaning both eyes do not work together. It may result from long-untreated intermittent exotropia or be present from early stages. Common signs include persistent double vision, reduced depth perception, and a habit of turning the head to align objects.
- Congenital (Infantile) Exotropia: Appears before 6 months of age and is often linked to neurological conditions or significant developmental disorders. Both eyes may drift outward noticeably and continuously. It’s commonly associated with delays in motor and visual development. This type requires early and aggressive treatment to prevent long-term vision loss.
- Sensory Exotropia: Caused by a significant loss of vision in one eye, which leads to a loss of normal binocular vision. The good eye becomes dominant, and the weaker eye drifts outward. It can occur at any age but is more common after age 5. Often accompanied by a history of eye trauma, retinal disease, or severe amblyopia. Patients may not notice symptoms until it becomes cosmetically evident.
How Is Exotropia Diagnosed?
Diagnosis is usually done by a pediatric ophthalmologist or an optometrist using a range of tools. Below is an overview of the main diagnostic methods, their accuracy, and average cost.
| Diagnostic Method | Accuracy (1–10) | Avg. Cost (USD) |
|---|---|---|
| Cover-Uncover Test | 9 | $100–$200 |
| Hirschberg Test | 8 | $50–$100 |
| Prism Test | 9 | $150–$250 |
| Visual Acuity Test | 8 | $75–150 |
| MRI/CT Scan | 10 | $1,000–$3,000 |
Cover-Uncover Test
This is one of the simplest and most frequently used methods to detect exotropia or wall eyes. The doctor covers one eye and observes the movement of the other. If the uncovered eye shifts to re-fixate on an object, it signals a misalignment. The test is non-invasive, takes less than a minute, and is usually comfortable for both children and adults. Results are immediate, making it a quick screening tool with high accuracy.
Hirschberg Test
A classic yet reliable examination, the Hirschberg Test involves shining a light into the patient’s eyes and observing where the reflection falls on the cornea. For patients with exotropia, the reflection appears off-center, confirming outward deviation. The process is completely painless and takes under two minutes. Although its precision depends on the examiner’s experience, it remains one of the fastest ways to identify wall eyes in infants and toddlers.
Prism Test
This test helps quantify the exact degree of eye deviation. The examiner places prisms of varying strength before one eye until alignment appears normal. It is slightly more complex and may take around 10–15 minutes, depending on cooperation and severity of misalignment. The test is safe and comfortable, though it requires professional skill to interpret results accurately.
Visual Acuity Test
While this test is widely known for measuring clarity of vision, it also aids in detecting whether vision imbalance may contribute to exotropia. Patients are asked to read letters or recognize symbols at varying distances. The test takes about five minutes, is non-invasive, and provides instant results. It helps determine whether reduced vision in one eye could be causing or worsening wall eyes.
MRI/CT Scan
This advanced imaging method is used only when a neurological cause is suspected. MRI or CT scanning reveals whether brain or nerve abnormalities are affecting the eye muscles. The procedure is entirely painless but can be intimidating for some patients due to the enclosed scanner and duration (20–40 minutes). Results are typically ready within a day. Despite its high cost, it provides the most detailed insight and near-perfect diagnostic accuracy.
Modern Treatments and Technologies
Treatment varies depending on the severity and type of exotropia:
Non-Surgical Treatments
- Corrective Glasses: Especially effective for cases linked to refractive errors. Glasses have a high compliance rate among children and cost between $150–$300. They are often the first step in treatment.
- Vision Therapy: Computer-based and in-office exercises to improve binocular vision. Brands like Vivid Vision and OptoPlus are gaining popularity. Therapy effectiveness ranges from 60–75%, especially for intermittent exotropia. Costs vary from $1,500–$5,000 for multi-session programs. This approach is widely recommended for children as a non-invasive option.
- Eye Patching: Helps strengthen the weaker eye and improve fusion control. Patches cost around $20–$50 per month. This is most often recommended in early or mild cases, or alongside vision therapy.
- Botox Injections: Temporarily paralyzes overactive muscles. Results last 3–6 months and may require repeated treatments. Each injection costs approximately $400–$800. Botox is mainly used for adults or as a short-term alternative before surgery. Effectiveness is moderate (around 50–60%) but improves alignment for some.

Surgical Options
Surgery becomes necessary if non-invasive methods fail:
- Strabismus Surgery: Muscles are repositioned to align the eyes. Recovery time is usually 2–4 weeks. Costs range from $4,000–$7,000 per eye. Success rates are high—estimated 80–90% for well-selected cases. This is the most commonly chosen method for constant exotropia and late-stage intermittent cases.
- Adjustable Suture Surgery: Allows fine-tuning post-operation. Commonly used in adult cases to improve precision. Slightly more expensive—averaging $6,000–$8,000—but offers better postoperative alignment control. Often chosen when exact alignment is critical or previous surgeries have failed.
Case Example: A 9-year-old girl from Chicago underwent strabismus surgery after vision therapy proved insufficient. Six months later, her alignment was stable with no recurrence.
Annual Number of Exotropia Surgeries by Country (2023)
This chart displays the number of exotropia surgeries performed in 2023 across various countries. India leads with 18,000 surgeries, followed by China and the USA, while Brazil and the UK report comparatively lower surgical volumes.
Prognosis and Outcomes
With early detection and appropriate treatment, 85–90% of patients experience significant improvement. Intermittent exotropia in children often has the best outcome when treated before age 7.
Living with Exotropia
Living with exotropia goes beyond managing the physical alignment of the eyes—it involves emotional, social, and practical adjustments. Individuals, especially children, might experience self-consciousness or be misunderstood in social situations. Managing daily routines with intention can significantly improve comfort and confidence.
Lifestyle Adaptations
Creating a structured daily routine that includes visual breaks, scheduled therapy sessions, and low-stress periods is essential. Overstimulation can intensify symptoms, so calming environments and sufficient sleep are highly beneficial.
Nutrition and Hydration
A diet rich in antioxidants and eye-supporting nutrients such as lutein, zeaxanthin, omega-3 fatty acids, and vitamins A, C, and E supports eye health. Staying hydrated helps maintain optimal tear film, which can ease eye fatigue.
Eye Hygiene and Comfort
Avoid touching or rubbing the eyes, as this can irritate already sensitive muscles and strain coordination. Use artificial tears if dryness or discomfort occurs. Blue light glasses may help those spending extended periods on digital devices.
Support Systems and Communication
For children, parental reassurance and teacher awareness are key. For adults, informing colleagues and using simple communication about the condition can reduce social anxiety. Support groups and online communities can also offer valuable encouragement.
Vision Exercises at Home
Simple convergence and divergence exercises done daily can maintain therapy progress. Use a pencil or finger to slowly move from arm’s length toward the nose, focusing both eyes together.
Quick Tips for Daily Life
- Use proper lighting for reading: Poor lighting can cause eye strain and worsen focus. Ensure that reading areas are well-lit with warm, indirect lighting. Avoid screen glare by adjusting screen brightness and using anti-glare filters if needed.
- Encourage kids to take screen breaks every 20 minutes: Implement the 20-20-20 rule—every 20 minutes, look at something 20 feet away for at least 20 seconds. Set reminders or use screen break apps to build this habit.
- Regular checkups with an ophthalmologist—at least once a year: Routine visits help monitor eye alignment and detect early signs of progression. Keep a journal of symptoms or eye behaviors to share with the specialist during visits.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends early screening by age 3—especially if there’s a family history of eye misalignment. He also emphasizes that combining vision therapy with lifestyle adjustments provides the best long-term results. “Don’t wait for the symptoms to become obvious. If one eye starts drifting even occasionally, get it checked—early intervention changes everything,” he advises.
Patients are encouraged to choose clinics with pediatric ophthalmology specialization and modern therapy programs.
References
- American Association for Pediatric Ophthalmology and Strabismus (AAPOS)
https://aapos.org
Source for statistical data on prevalence, gender ratios, and treatment trends. - JAMA Ophthalmology, 2021 Study on Pediatric Eye Disorders
https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2777739
Cited for the 35% increased risk of strabismus in children with delayed visual development. - National Eye Institute (NEI)
https://nei.nih.gov
Referenced for general definitions, symptoms, and causes of exotropia. - American Optometric Association (AOA)
https://aoa.org
Provided data on diagnosis methods, visual testing standards, and therapy recommendations. - PubMed Central / NCBI
https://www.ncbi.nlm.nih.gov/pmc
Source for data supporting Botox use and outcomes in strabismus treatment. - Vision Therapy: Vivid Vision and OptoPlus Clinical Data
https://www.seevividly.com | https://www.optoplus.com
Referenced for therapy success rates, program costs, and technological approaches. - Strabismus Surgery Cost Data – HealthCare Bluebook
https://healthcarebluebook.com
Used to estimate cost ranges and common outcomes for strabismus-related procedures. - Centers for Disease Control and Prevention (CDC)
https://www.cdc.gov
Provided supplemental context for developmental risk factors (e.g., premature birth). - Botulinum Toxin Use in Ophthalmology – Review Article
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3550221
Cited for temporary effect duration, usage frequency, and effectiveness data. - Mayo Clinic – Eye Misalignment and Strabismus Resource
https://www.mayoclinic.org/diseases-conditions/strabismus
General overview of diagnosis, types, and patient-friendly descriptions.



