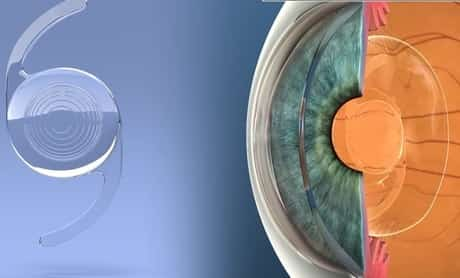
How multifocal IOLs with lower add powers might be better to patients than higher-add lenses. Astronomers sometimes describe the area in our solar system occupied by the Earth as the “Goldilocks Zone”: Its range from the Sun makes it neither too hot nor too cold to support liquid water; but instead, it’s ideal. Cataract surgeons are beginning to think there might be a Goldilocks zone for many patients who are prospects for multifocal intraocular lenses, too, other than in this case it’s around the distance of a car’s control panel or a home computer. If the add power’s centerpiece is any better, some surgeons say, the client doesn’t have a much intermediate vision at all.
In this short article, surgeons talk about the benefits of low- and mid-add multifocal lenses, and why they may be more appealing alternatives for patients than lenses with higher add powers.
How Are Using Multifocal Lens?
Surgeons state is implanting a high-add multifocal, such as a +4D, would often take a great deal of modification on the patient’s part.
“With the initial, higher-add lenses, I’d routinely counsel patients about the centerpiece of the include,” remembers Bakersfield, Calif., surgeon Daniel Chang. “Particularly for patients who were more youthful and still working and/or utilizing the computer system a lot, that intermediate computer system variety was not at the lens’s best focal point. I ‘d let them know they might have to adjust where their computer system screen sat. To take a look at the computer system at the back of their desk, there was a dip in the vision at that range, and it would be blurrier. The high-add lenses had an optimal centerpiece of about 14 inches, but, functionally, many things in patients’ lives was beyond that, more in the 20-inch variety.”
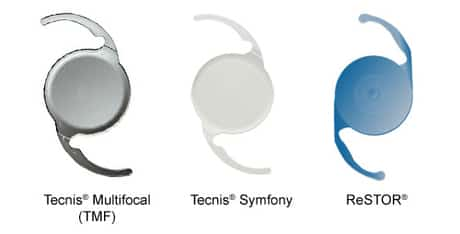
Iselin, N.J., ophthalmologist Doug Grayson states the high-add patients’ visual needs would often confuse even health-care personnel. “When we were implanting the [Tecnis] ZMB00, they ‘d lose the intermediate zone of vision,” he states. “If patients needed computer vision, we were giving them -1D glasses to bring their vision out a little farther. That was the only solution. Some referring optometrists didn’t comprehend the principle that they were handling a multifocal that had almost too-high of an add power. They were offering these patients +1D reading glasses for the computer, but the idea is that you have to decrease the include for that distance. So, I ‘d end up calling them and asking them to give the patients a -1D phenomenon.”
What Type of Multifocal Lenses Surgeons Recommend to Patients
Surgeons state the more recent add powers in the middle and low range bring many advantages.
– The intermediate centerpiece. Los Altos, Calif., surgeon Bryan Lee states low- and mid-power includes mesh better with lots of patients’ activities. “Compared to the stronger-add multifocals, the lower includes offer patients a lot more intermediate vision,” he states. “Our world has changed. There are a lot more things today that we use our intermediate vision for than we used to, specifically when you think about the tablet, desktop and notebook computer, which are even being utilized more regularly by our cataract-age patients. Patients want to trade a little small print reading ability for much better intermediate vision. Also, a low- or mid-add does not simply enhance their practical vision; it also gives a more constant variety of vision.”
Jeffersonville, Ind., ophthalmologist Asim Piracha says this smoother shift between intermediate and far vision in the low add powers is an outcome of pushing the centerpiece out a little further. “I think about the mid- and low-add multifocal IOLs as kind of progressive lenses vs. the high-adds, which are more like bifocals,” he states. “With the high-add, you come up to, and you get far, and nothing else. Also, it’s a truly close near, so the intermediate to far-intermediate vision merely is gone. This is why the patients with +4D multifocals will require computer system glasses. So the near vision is terrific; however, the general vision isn’t very functional for lots of patients with a high-add lens. The low-add patients get intermediate to near vision, and they can see beyond arm’s length, so it’s suitable for phones, iPads, computers, laptops, the table, vehicle control panels, and so on. It’s a variety of vision, while previously, with a high-add, it was more like a bifocal, where you ‘d have near, and then it would just drop off, and then you ‘d have range vision.
Other review: “The other thing is, there’s more space for the mistake with the low-add lens,” Dr. Piracha adds. “So if a low-add patient is ± 0.5 D postop, particularly if it’s -0.5D, he’s quite pleased since he’ll have good range vision, perhaps 20/30, and still have good near. Since of this, I’ve been trying to target about -0.25 D on these low adds, so if I’m off, I’ll be off a bit on the minus side, and they’ll still more than happy with their range vision. This is various from the high-add lenses, such as the +4 D, where if the patient isn’t perfectly plano he’s dissatisfied.”
Dr. Chang says the concept of needing glasses to check out some fine print or perform near jobs appears to sit better with patients than having an abrupt drop in vision in between near and far. “I’ll counsel the low-add patients that they’ll still need glasses for excellent print, and the FDA data reveals that,” he explains. “For them, it makes good sense to require reading glasses sometimes for small print, but to have a drop-off in their vision at the intermediate range, as holds with the high-add lenses, does not make as much sense, and is a bit harder to handle.”
In regards to binocular uncorrected visual results, in the Food and Drug Administration study of the AcrySof IQ ReSTOR 2.5 D lens, patients saw approximately 0.01 logMAR at range (around 20/20+), 0.25 at intermediate (between 20/30 and 20/40) and 0.34 at near (in between 20/40 and 20/50).1 In the FDA study of the Tecnis 2.75-D (ZKB00) and 3.25-D (ZLB00) multifocals, 93 percent of the 2.75-D eyes and 96 percent of the 3.25-D eyes attained 20/40 or better-uncorrected range vision monocularly. In regards to binocular uncorrected near acuity (40 cm), 95 percent of the 2.75-D eyes and 99 percent of the 3.25-D eyes saw 20/40 or much better at six months.2 When taking a look at the lenses’ focal points, in addition to having a sharp vision in the distance, on the defocus curve the 2.75-D lens peaked at 50 cm (intermediate distance) and the 3.25-D lens peaked at a closer 40 cm.
Diminished halos and night-vision problems. In some sense, this advantage of the low- and mid-add lenses could be a bigger boon to patients than enhanced intermediate vision, considering that it makes the lenses more bearable for the client and less problematic for surgeons to manage postop.
Tecnis Multifocal Lens Review

Surgeons have noticed that patients complain less about night-vision problems, glare and halos with lower-add multifocal lenses, and the information bears this out. In the FDA research study of the Tecnis 2.75 D for example, the lens had fewer night-vision complaints than the 3.25-D. Interestingly, it also had fewer night-vision grievances than the Tecnis monofocal control lens: 8.5 percent of 2.75-D patients reported moderate trouble seeing at night vs. 9.7 percent with the monofocal, and just 0.7 percent reported severe difficulty vs. 4.1 percent with the monofocal IOL. Though the ReSTOR 2.5-D trial didn’t take a look at night-vision issues, the lens did publish a somewhat lower portion of moderate and extreme glare problems than the 4D 1,3.
Dr. Chang states that, on the 2.75-D Tecnis, the halos are merely smaller than on higher-add variations. “The halo that the patient sees is the energy directed towards the near focal point,” he describes. “So, when you’re taking a look at a remote point source of light, it’s out of focus and is instead focused on the retina as a halo. So, the higher your include the lens, the larger your halo. In other words, the 4-D Tecnis has a particular size halo, the 3.25-D has a smaller halo, and the 2.75-D has an even smaller sized halo. In fact, in the past, when patients with higher-add multifocals in my practice would grumble about halos, it usually was because of the halo’s size instead of its brightness. Specifically, they ‘d grumble that the halo was too big and that it was obstructing their view of cars coming towards them during the night. So, the low-add multifocals make these halos smaller. If you look at the night-vision complaint statistics on the Tecnis package insert, the halo complaints get progressively smaller size as the included power declines. There was even less difficulty in the evening with the low-add multifocal than with the monofocal control in the FDA approval information. That’s unexpected. By the method of explanation, I think that, for patients, the advantage of having some include power that permits them to see their dashboard at night surpasses the drawback that halos produce. In truth, if you take a look at the halo data as a separated grievance with the 2.75-D multifocal, it was higher than with the monofocal– however patient satisfaction was higher, and night-vision problems were lower. I think if you look at the big image, people like the low include.
“I’d prefer to cause fewer night-vision symptoms in patients and have near vision that wasn’t rather as sharp, because you can utilize checking out glasses for the up-close things if you wish to see them,” Dr. Chang continues. “But, you can’t amazingly make halos and night-vision problems disappear.”
ReSTOR Multifocal Lens Review
Surgeons say the improvement in visual grievances is an outcome of both style components, and the lower power includes resulting in a smaller diffractive impact (i.e., less diffractive rings on the IOL), which equates into fewer visual problems. “In the ReSTOR lens in specific, the central element has fewer rings,” discusses Bret Fisher, MD, of Panama City, Fla. “And the overall diffractive area of the lens is smaller compared to the 3-D add. There’s also a new main refractive zone, along with a bigger peripheral refractive zone, both utilized for range vision. The combination of fewer rings and the existence of these refractive zones acts to lessen the dysphotopsias patients have at night.”
Patients Reviews and Choice
Though the low-add multifocals can be useful for lots of patients, surgeons state you still need to do your due diligence ahead of time to pick the right lens — or perhaps even mix two include powers– to get the very best results.
Dr. Piracha makes sure to have a thorough conversation with the client about his occupation and any hobbies. “I have implanted a couple of Tecnis 3.25-D lenses; however, 95 percent are the 2.75 D,” he states. “The ones for whom I advise the 3.25 are those who state they check out all the time, or ‘I wish to read in bed,’ or ‘I wish to have the ability to check out a book, but I’m not on the computer system that much,’ or the client who says he likes to hold things up close while doing great needlework or woodworking. These are generally the older patients; the very same patients who would have done fine with the 4 D will do even much better with the 3.25 D. However, if they mostly utilize the intermediate distance, such as dealing with the computer system, or if they’re a chauffeur by trade and night vision is necessary to them, I’ll utilize the low-add lens. Many of my patients like to shoot rifles, so what’s nice with the low-add lens is they can see both the target and the weapon sight at the same time. That’s something monovision can’t do. Among my patients owns his shooting range, contends professionally and trains kids, and he’s thrilled with the low-add lens.” Some surgeons will likewise provide patients surveys about their activities to choose the right lens for them.
Dr. Chang likes to observe how the client reads firsthand. “I’ll hand him a pamphlet or some other instructional product for him to review and simply look at where he holds it,” he states. “I enjoy where he automatically holds it, whether it’s because of his glasses, his current prescription or whatever. I use that variable as a guide for which lens I’m going to start with. So, if he holds the product up close, then I’ll offer him a 3.25 D or potentially even a 4 D. If he holds it farther out, I’ll choose the 2.75-D add.”
A good variety of surgeons will attempt to get the very best of both worlds and will implant a low-power multifocal lens in one eye and in the other eye implant a multifocal lens with a slightly higher power to try to cover a larger focal variety. Milan’s Francesco Carones has blended low- and mid-add IOLs in 700 patients. In his cases, he generally blends a low-power 2.5-D ReSTOR with a 3-D ReSTOR, and he states it works well. “My personnel and I devote a lot of time to trying to find the best solution for each private client,” Dr. Carones says. “We also use activity surveys that ask such questions as how much time they’re using eyeglasses for certain activities, and the number of those activities would they like not to have to use spectacles. I’ve found that about 70 percent of my patients answer in manner ins which would indicate they ‘d do much better with a mixed technique. About 20 percent would do much better with a 3-D lens implanted bilaterally, and 10 percent would choose bilateral 2.5-D lenses.” He implants the low-add in the dominant eye when mixing.
Review from Dr. Carones: Dr. Carones studied the outcomes of this blending approach in 40 patients, comparing the outcomes to 20 patients who got bilateral 2.5-D ReSTORs. Postop, in the bilateral 2.5-D group, all patients were 20/20 uncorrected for distance, and all saw 20/20 or better uncorrected at intermediate (measured as 60 cm in the research study). Just six patients (30 percent) had 20/20 at 40 cm, while all saw at least 20/50 at that variety. In the combined group, Dr. Carones says you can see an expanded variety of vision at near: All might see 20/20 at the range. Ninety-three percent saw 20/20 or better at intermediate, and 70 percent saw 20/20 or better at near, with everybody in the group seeing at least 20/32 at near.
Lee’s review: In everyday practice, surgeons say this blending can frequently make sense for patients. “In the first eye, I generally implant the lowest include power,” says Dr. Lee. “I’ll then wait a bit longer than typical for the patient to recuperate given that it’s multifocal. That way, the patient has time to get used to the multifocal. When he returns for a postop check out, I’ll talk to him about the function of that first eye, asking such questions as, ‘Do you like it? Do you want the second eye to match it? Would you instead value having some more reading-distance vision in the second eye?'” If he states he ‘d prefer more checking out a vision, I’ll go for the intermediate power for the 2nd eye. For instance, if I’m using the Tecnis, I ‘d implant the 3.25-D include.”
Dr. Fisher explains: The low-add multifocals, such as the AcrySof ReSTOR he utilizes, can likewise work when paired with a monofocal IOL that the patient had implanted in the fellow eye years formerly. “I’ve done several patients who have had a monofocal IOL in one eye now for years,” he states. “I’ve been able to provide them a lower-add multifocal for the other eye, knowing that they wouldn’t feel as if they were compromising on the distance vision compared to their monofocal lens, which they were also getting some intermediate vision. I believe that highlights what a good ‘utility gamer’ these lenses are ending up being.”