Histoplasmosis is a disease triggered when airborne spores of the fungus Histoplasma capsulatum are breathed in into the lungs, the main infection site. This microscopic fungus, which is discovered throughout the world in river valleys and soil where bird or bat droppings collect, is released into the air when soil is disrupted by plowing fields, sweeping chicken coops, or digging holes.
Histoplasmosis is frequently so moderate that it produces no evident symptoms. Any symptoms that may occur are often much like those from an acute rhinitis. In reality, if you had histoplasmosis symptoms, you might dismiss them as those from a cold or flu, considering that the body’s body immune system typically gets rid of the infection in a couple of days without treatment.
Nevertheless, histoplasmosis, even mild cases, can later cause a major eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
What Causes Ocular Histoplasmosis Syndrome
Scientists believe that Histoplasma capsulatum (histo) spores spread out from the lungs to the eye, accommodations in the choroid, a layer of blood vessels that supplies blood and nutrients to the retina. The retina is the light-sensitive layer of tissue that lines the back of the eye. Scientists have actually not yet had the ability to spot any trace of the histo fungus in the eyes of patients with ocular histoplasmosis syndrome. Nevertheless, there readies reason to believe the histo organism as the cause of OHS.
Ocular Histoplasmosis Development in Humans
OHS establishes when vulnerable, abnormal blood vessels grow underneath the retina. These irregular blood vessels form a lesion called choroidal neovascularization (CNV). If left without treatment, the CNV lesion can develop into scar tissue and replace the normal retinal tissue in the macula. The macula is the main part of the retina that provides the sharp, main vision that permits us to read a newspaper or drive a cars and truck. When this scar tissue types, visual messages from the retina to the brain are impacted, and vision loss outcomes.
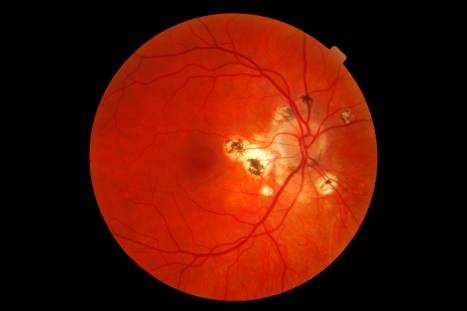
Vision is likewise impaired when these abnormal capillary leak fluid and blood into the macula. If these irregular blood vessels grow towards the center of the macula, they may impact a small depression called the fovea. The fovea is the region of the retina with the highest concentration of unique retinal afferent neuron, called cones, that produce sharp, daytime vision. Damage to the fovea and the cones can severely impair, as well as damage, this straight-ahead vision. Early treatment of OHS is essential; if the abnormal capillary have actually impacted the fovea, managing the disease will be more difficult. Given that OHS hardly ever impacts side, or peripheral vision, the disease does not cause total blindness.
Who Is at Risk for Ocular Histoplasmosis Syndrome?
Although only a small fraction of individuals infected with the histo fungus ever establishes OHS, any person who has had histoplasmosis should be alert for any changes in vision much like those described above. Studies have shown the OHS patients usually test positive for previous exposure to histoplasmosis.
In the United States, the highest incidence of histoplasmosis occurs in a region frequently described as the “Histo Belt,” where up to 90 percent of the adult population has been infected by histoplasmosis. This area includes all Arkansas, Kentucky, Missouri, Tennessee, and West Virginia in addition to large parts of Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana, Maryland, Mississippi, Nebraska, Ohio, Oklahoma, Texas, and Virginia. Because many cases of histoplasmosis are undiagnosed, anybody who has actually ever resided in an area understood to have a high rate of histoplasmosis should think about having their eyes examined for histo spots.
Symptoms of Ocular Histoplasmosis Syndrome
Ocular Histoplasmosis Syndrome generally has no symptoms in its early stages; the preliminary OHS infection usually subsides without the need for treatment. This is true for other histo infections; in truth, frequently the only proof that the inflammation ever happened are small scars called “histo spots,” which stay at the infection sites. Histo spots do not usually affect vision, but for factors that are still not well understood, they can lead to complications years– sometimes even decades– after the initial eye infection. Histo spots have been associated with the development of the irregular blood vessels below the retina.
In later stages, Ocular Histoplasmosis Syndrome symptoms may appear if the abnormal blood vessels cause modifications in vision. For example, straight lines might appear misaligned or wavy, or a blind spot might appear in the field of vision. Since these symptoms show that OHS has actually currently advanced enough to impact vision, anybody who has been exposed to histoplasmosis and perceives even small modifications in vision should seek advice from an eye care specialist.
How Is Ocular Histoplasmosis Syndrome Diagnosed?
An eye care professional will usually detect OHS if a cautious eye examination exposes two conditions: (1) The existence of histo spots, which show previous direct exposure to the histo fungus spores; and (2) Swelling of the retina, which signifies the development of brand-new, abnormal capillary. To validate the medical diagnosis, a dilated eye examination should be performed. This means that the pupils are enlarged temporarily with unique drops, enabling the eye care professional to better examine the retina.
If fluid, blood, or abnormal blood vessels exist, an eye care expert might want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient’s arm, travels to the blood vessels of the retina. The color permits a better view of the CNV sore, and photos can record the area and level to which it has actually spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
Treatment for Ocular Histoplasmosis Syndrome
The only proven treatment for OHS is a form of laser surgery called photocoagulation. A little, effective beam destroys the delicate, irregular blood vessels, in addition to a percentage of the overlying retinal tissue. Although the destruction of retinal tissue during the procedure can itself cause some loss of vision, this is done in the hope of protecting the fovea and preserving the finely-tuned vision it provides.
How effective is laser surgery?
Controlled clinical trials, sponsored by the National Eye Institute, have actually shown that photocoagulation can lower future vision loss from OHS by over half. The treatment is most effective when:
- The CNV has actually not grown into the center of the fovea, where it can affect vision.
- The eye care professional has the ability to determine and destroy the entire area of CNV.
Does laser surgery bring back lost vision?
Laser photocoagulation normally does not restore lost vision. Nevertheless, it does decrease the possibility of more CNV growth and any resulting vision loss.
Does laser surgery cure Ocular Histoplasmosis Syndrome?
No. OHS can not be treated. Once contracted, OHS stays a hazard to a person’s sight for their lifetime.
People with OHS who experience one bout of abnormal blood vessel growth may have recurrent CNV. Each reoccurrence can damage vision and might require extra laser therapy. It is vital to spot and treat OHS as early as possible before it causes considerable visual disability.
Is there a basic way to look for signs of OHS damage to the macula?
Yes. A person can look for signs of damage to the macula by looking at a printed pattern called an Amsler grid. If the macula has been harmed, the vertical and horizontal lines of the grid may appear curved, or a blank spot may appear to appear.
Numerous eye care specialists recommend patients who have actually received treatment for OHS, in addition to those with histo spots, to check their vision daily with the Amsler grid one eye at a time. Patients with OHS in one eye are likely to establish it in the other.
What help is offered for people who have already lost significant vision from OHS?
Scientists and engineers have actually established numerous helpful devices to help people with severe visual problems in both eyes. These devices, called low vision aids, use special lenses or electronic devices to create enlarged visual images. An eye care specialist can recommend sources that provide information on therapy, training, and unique services for people with low vision. Lots of companies for people who are blind also serve those with low vision.