Ocular migraines, also known as retinal migraines, are a rare type of migraine that causes visual disturbances in one eye, such as flashing lights, blind spots, or even temporary vision loss. These episodes usually last between a few minutes to an hour and are often followed by a headache, but not always.
Most Common Symptoms Reported During Ocular Migraines
This chart displays the most common symptoms experienced during ocular migraines. Visual disturbances were reported most frequently, followed by temporary vision loss and post-aura headaches. The data helps highlight the range and prevalence of symptoms associated with this condition.
How Do Ocular Migraines Differ From Visual Migraines?
This is one of the most common points of confusion. Visual migraines affect both eyes and typically involve shimmering zigzag patterns or kaleidoscope-like distortions. Ocular migraines, on the other hand, affect only one eye and may lead to partial or complete temporary vision loss. A simple way to test: cover one eye at a time during an episode. If the disturbance is still there regardless of which eye is closed, it’s probably a visual migraine.
What Are the Symptoms of an Ocular Migraine?
Symptoms may vary but generally include:
- Temporary vision loss in one eye
- Flickering or flashing lights
- Blind spots (scotomas)
- Nausea or light sensitivity
- Headache (not always present)
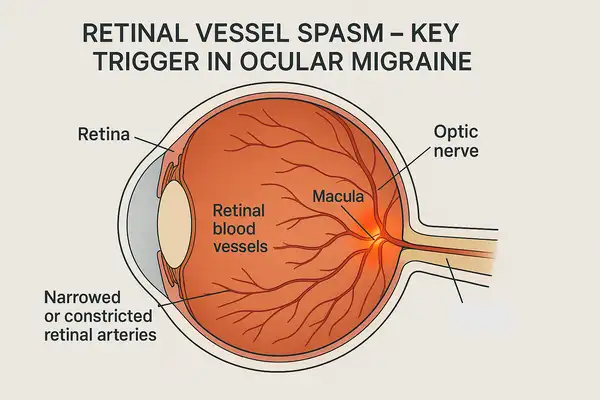
What Causes Ocular Migraines?
Ocular migraines are believed to be caused by spasms or sudden constrictions in the blood vessels of the retina. Triggers may include:
- Stress and fatigue: Mental or emotional stress—such as preparing for a deadline, job interviews, or arguments—can lead to ocular migraines by increasing cortisol levels and disturbing blood flow to the retina. Physical fatigue from intense exercise, manual labor, or extended driving can also contribute, especially when paired with dehydration or inadequate rest. Many patients report episodes after long workdays or disrupted sleep schedules.
- Bright or flickering lights: Exposure to high-intensity lighting or prolonged screen time can overstimulate the retina. Common situations include night driving, working under fluorescent lights, or gaming on high-contrast screens. Photostimulation disrupts the retinal vasculature in sensitive individuals, often leading to an episode within minutes to an hour of exposure.
- Hormonal fluctuations: Hormonal changes—particularly estrogen level shifts during menstruation, pregnancy, or menopause—can affect vascular tone and are frequently linked to ocular migraines in women. Episodes are most likely to occur during the days leading up to menstruation or during the early postpartum period.
- Certain foods: High-tyramine foods like aged cheese, processed meats, and red wine may lead to retinal vessel constriction. These dietary triggers typically induce symptoms within 30 minutes to a few hours after consumption. Caffeine overuse or sudden withdrawal can have a similar effect.
- Dehydration: Even mild dehydration (loss of 1–2% body weight in fluids) can reduce blood volume and affect cerebral and retinal circulation. Situations include hot weather, vigorous exercise without fluid replacement, or long periods without drinking water. This is one of the most underestimated and preventable triggers.
- High blood pressure: Acute spikes in blood pressure—especially during emotional distress or physical exertion—can lead to temporary disturbances in retinal perfusion. This is most common in patients with uncontrolled hypertension, often manifesting early in the morning or during moments of anxiety.
Understanding these triggers helps in developing an effective management plan. Most patients benefit from identifying their most sensitive conditions and adjusting habits accordingly.
How Are Ocular Migraines Diagnosed?
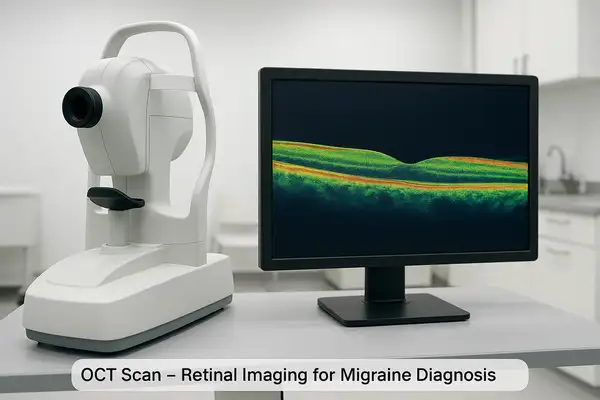
Diagnosing ocular migraines involves a combination of clinical evaluation, patient history, and diagnostic tests to rule out other serious conditions such as retinal detachment or stroke. Common diagnostics include:
| Diagnostic Method | Description | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|---|
| Eye Exam | Assesses retinal health | 7/10 | $100–$250 |
| Optical Coherence Tomography (OCT) | Cross-sectional retinal imaging | 9/10 | $150–$500 |
| MRI/CT Scan | Rules out neurological causes | 9/10 | $500–$3,000 |
| Visual Field Test | Maps visual blind spots | 8/10 | $75–$200 |
Can Ocular Migraines Indicate Something More Serious?
Occasionally, yes. If symptoms are frequent or worsening, or if vision loss lasts more than an hour, it could point to underlying vascular or neurological issues. Immediate consultation with a neurologist or ophthalmologist is recommended.
What Are the Treatment Options?
Treatment is typically preventive and focused on managing triggers. Medications used include:
- Beta-blockers such as Inderal LA (propranolol), commonly prescribed for cardiovascular conditions and migraine prevention. Average effectiveness: 6–8/10 depending on patient history.
- Calcium channel blockers like Calan SR (verapamil), effective in reducing frequency of migraine episodes, especially when related to vascular spasms. Effectiveness rating: 7/10.
- Anti-seizure medications including Topamax (topiramate), often prescribed off-label for migraine prevention. Notably effective in chronic cases. Success rate: up to 80% reduction in frequency for some users.
- Triptans such as Imitrex (sumatriptan) or Maxalt (rizatriptan) are used when ocular migraines are followed by intense headache. These are abortive, not preventive, and should be taken at onset. Effectiveness: 7–9/10 for pain and aura mitigation.
Most of these medications are used long-term and may require several weeks for full therapeutic effect. Physicians in the U.S. typically start with lower doses to minimize side effects such as fatigue, dizziness, or mood changes.
Effectiveness of Common Treatments for Ocular Migraines
This chart presents the reported effectiveness of various treatments for ocular migraines. Resting in a dark room and prescription medication appear to be the most effective options, while simpler remedies like hydration and cold compress provide limited relief for most individuals.
Advanced and Assistive Technology
For patients with frequent episodes, wearable technology can be a game changer:
- Smartwatches like Apple Watch or Fitbit can monitor heart rate variability and stress levels, helping detect patterns.
- Blue light filtering glasses (e.g., from brands like Felix Gray or Gunnar) reduce exposure to visual triggers, especially during extended screen use.
- Continuous blood pressure monitors can help correlate hypertensive episodes with migraine onset.
Combination Strategies
Many neurologists recommend combining pharmacological therapy with lifestyle management. For example, a patient on low-dose verapamil may achieve even better control when they adopt hydration routines and reduce screen time.
Real Medical Example: A 38-year-old female from Chicago experienced weekly vision loss episodes in her right eye. After using a blue light filtering lens and adjusting her diet to avoid high-tyramine foods, the episodes reduced to less than once per month. Later, her physician introduced low-dose topiramate, and she has remained symptom-free for three months.
In summary, treatment success relies on accurate diagnosis, trigger awareness, and an individualized regimen that may include both medication and tech-based solutions.
Are There Any Lifestyle Changes That Help?
Absolutely. While medication plays a role, lifestyle modifications can significantly reduce frequency and severity:
- Regular sleep schedule
- Hydration (2–3 L/day or 68–101 oz)
- Low-tyramine diet
- Screen time breaks
- Use of anti-glare screens or eyewear
When and for Whom Are These Changes Most Effective?
Lifestyle changes are most beneficial for individuals who:
- Experience mild to moderate ocular migraines
- Have identifiable triggers (e.g., stress, dehydration, visual strain)
- Prefer a preventive approach over chronic medication
- Are ineligible for or wish to avoid pharmacological treatment
These measures are particularly effective when migraines are infrequent but disruptive. In patients with a strong correlation to diet or sleep habits, lifestyle changes alone may reduce episodes by 60–80%.
How to Combine Them for Better Results
Combining several strategies enhances the effect. For example:
- Use a hydration reminder app + follow a low-tyramine meal plan
- Apply the 20-20-20 rule for screen breaks + wear blue light filtering glasses
- Maintain a sleep journal + limit caffeine intake after 2 PM
Expected Outcomes
Depending on adherence, patients often report:
- Fewer episodes within 2–4 weeks
- Milder symptoms when migraines do occur
- Improved energy levels and concentration
Real-Life Insight
One 42-year-old male patient from Seattle reduced ocular migraine episodes from 5 per month to 1 per month after integrating regular hydration, a Mediterranean-style diet, and digital detox weekends.
In general, these strategies are low-cost, low-risk, and high-impact—perfect for those seeking a holistic, science-backed approach to managing ocular migraines.
Can Children Experience Ocular Migraines?
Yes, though it’s rare. Pediatric ocular migraines are often misdiagnosed as vision problems or even attention disorders. Any recurring visual disturbance in children warrants thorough neurological and ophthalmologic evaluation.
Children may not always be able to articulate what they’re experiencing, which can make diagnosis tricky. Parents might notice that a child suddenly stops playing, rubs one eye, or complains about “seeing stars” or “colors.” Some kids might describe vision that “fades” or becomes “wavy,” and others might say they feel dizzy or want to lie down in a dark room.
Typical complaints from children include:
- “I can’t see out of one eye.”
- “There’s a bright spot and I can’t see around it.”
- “It looks like everything is flashing.”
- “My head hurts and the lights are too bright.”
Ocular migraines in children can also be triggered by long screen time sessions, dehydration, lack of sleep, or stress — especially from academic pressure. One real example: a 10-year-old boy from Phoenix began experiencing brief vision loss in his left eye during math class. Doctors traced it to ocular migraines triggered by screen overuse and poor hydration. With schedule adjustments and blue-light glasses, the episodes were nearly eliminated.
In short, if a child repeatedly reports strange visual experiences, it’s crucial not to dismiss them as imagination or attention-seeking. A proper evaluation can prevent misdiagnosis and help manage symptoms effectively.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends that anyone experiencing recurrent visual disturbances—even if short-lived—should not brush them off. “The eye is an extension of the brain. A symptom in your vision could be a message from your nervous system. Get it checked,” he advises. Our editorial team suggests keeping a migraine diary, tracking diet, sleep, and symptoms. A proactive approach can dramatically improve quality of life.
Occupations Reporting the Highest Rates of Ocular Migraines
| Occupation | Affected Workers (%) |
|---|---|
| IT/Tech Workers | 18% |
| Healthcare Professionals | 15% |
| Teachers | 13% |
| Office Administrators | 10% |
| Retail Workers | 7% |
| Manual Laborers | 5% |
This chart outlines which occupations report the highest incidence of ocular migraines. IT and healthcare professionals appear most affected, possibly due to screen exposure and high-stress environments. The data suggests a correlation between cognitive workload and ocular migraine prevalence.
References
- American Migraine Foundation. What Is an Ocular Migraine? Available at: https://americanmigrainefoundation.org/resource-library/ocular-migraine/
- Mayo Clinic. Migraine with Aura. Available at: https://www.mayoclinic.org/diseases-conditions/migraine-with-aura/symptoms-causes
- National Eye Institute. Facts About Migraines and Visual Disturbances. Available at: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/migraines
- Cleveland Clinic. Ocular Migraine. Available at: https://my.clevelandclinic.org/health/diseases/17954-ocular-migraine
- MedlinePlus. Retinal Migraine. Available at: https://medlineplus.gov/ency/article/000709.htm
- Journal of Headache and Pain. Clinical features and management of visual aura in migraine. Available at: https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-021-01299-5