Optic neuritis is swelling of the optic nerve, triggered by damage to and loss of the protective sheath (myelin) surrounding this nerve that is so crucial for good vision. Demyelinating optic neuritis is another term for this eye condition.
Vision symptoms from optic neuritis can consist of blurring and blind spots. You likewise might notice distorted vision, decreased color vision and pain when you move your eyes. These types of symptoms may precede vision loss due to optic neuritis.
Optic neuropathy more usually describes optic nerve problems or damage, consisting of from causes such as blocked blood flow or harmful direct exposure.
What Causes Optic Neuritis?
Optic neuritis typically occurs in adults younger than 45 and affects more women than men. The condition prevails in people who have multiple sclerosis (MS), which takes place when the body’s own body immune system attacks and ruins protective nerve coverings.
Besides affecting vision, related nerve damage in MS can cause loss of mobility and sensory functions, along with other incapacitating conditions.
Other causes of optic neuritis and neuropathy include:
- Infections such as toxoplasmosis
- Ocular herpes
- Other viral infections
- Sinusitis
- Neurological conditions
- Leber genetic optic neuropathy, an acquired form of vision loss that affects primarily males in their 20s or 30s
- Nutritional deficiency
- Toxic substances, including alcohol and tobacco
During an eye examination, your optometrist will look for signs of optic neuritis by performing tests to examine whether you have reduced vision.
Your eye pressure will be measured, and your pupils will be dilated to provide a much better view of the eye’s interior structures, including the optic nerve and retina.
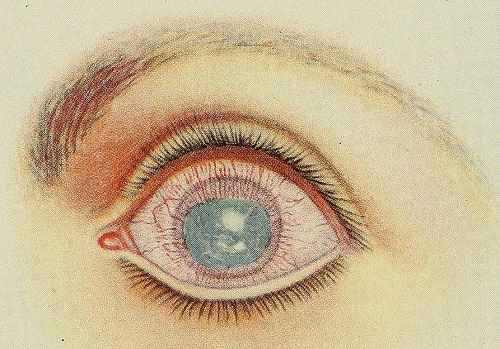
When optic neuritis is present, the pupil always appears unusual (afferent pupillary problem). This means the pupil in fact dilates instead of restricting in the presence of intense light. Depending upon the severity of optic neuritis, the optic nerve may appear normal or swollen.
If your optometrist or ophthalmologist suspects you have optic neuritis, a visual field test normally will be performed to identify if you have peripheral vision loss. You likewise might be described a specialized clinic to go through an MRI of the brain to spot possible underlying causes of optic nerve inflammation.
An individual with optic neuritis typically goes through an MRI of the brain, to search for main nerve system sores.
See also: Eye Pain: Inside, Around, Behind
Treatments For Optic Neuritis
Treatment of optic neuritis has changed over the last few years, due to a landmark series of studies known as the Optic Neuritis Treatment Trials (ONTT).
In these research studies, people with optic neuritis were randomized for treatment with intravenous (IV) steroids, oral steroids or placebo. Later they were evaluated for a number of years.
From these studies, scientists found out that treatment with steroids had little result on the last visual outcome in patients with optic neuritis.
Nevertheless, patients treated with IV steroids had less repeat attacks of optic neuritis than patients treated with oral steroids alone. In fact, those treated with oral steroids alone had a higher risk of repeat attacks of optic neuritis than those treated with placebo.
Even more notably, patients dealt with at first with IV steroids had about half the risk of developing MS in two years as patients treated with oral steroids only, or placebo. Of those treated with IV (followed by oral) steroids, 7.5 percent developed MS in the following two years, versus about 16 percent in the other groups.
As an outcome of the ONTT, optometrist now treat patients with a mix of IV and oral steroids or keep track of the condition without prescribing medical treatment. Use of oral steroids alone is not recommended.
For patients who are clinically treated, the regimen typically consists of three days of IV steroids, followed by about 11 days of oral steroids.
Also read: Eye Pain: Symptoms, Causes and Treatment
Prognosis For Those Who Have Optic Neuritis
Visual deficits brought on by optic neuritis may worsen over a duration of about seven days prior to vision normally supports at that level for 3 to 8 weeks. Gradual vision enhancement then might take place.
About 95 percent of people with optic neuritis will recover much of their vision within six months of start. Nevertheless, about 19 percent will have a reoccurrence of optic neuritis in the impacted eye, and 17 percent will establish optic neuritis in the other eye within 10 years.
As pointed out above, often optic neuritis is a precursor to development of MS, so if you have optic neuritis, your doctor may advise an MRI. If imaging shows “white matter” sores indicating damage to myelin in nerve fibers, there is a 56 percent opportunity of establishing MS within 10 years. However even with normal outcomes, a person with optic neuritis has a 22 percent opportunity of establishing MS.
My first Optic Neuritis event was about 20 years earlier. It was extremely tough to explain. At that time my description was that it was as if someone had erased parts of my visual field. There were no black holes just holes – areas where there was absolutely nothing. Obviously, there was the blurred vision but that was not nearly as annoying as those empty holes. Within a couple of months my vision was totally restored.
Then August of 2011 those darn holes were back. This time my eye doctor stated an MRI was essential. The rest is history officially after 20 years I had MS.
I have actually never experienced pain with the ON. My vision has not gone back to normal after this occasion. You just learn to compensate. I have great days and not so good days.