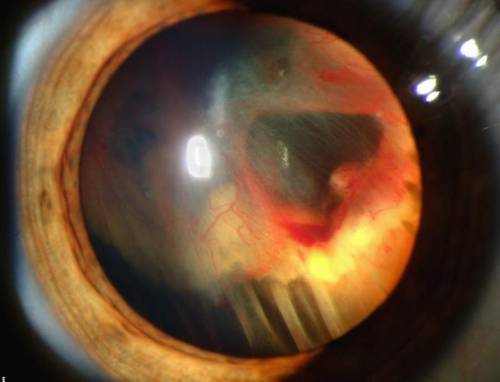
A detached retina happens when the retina peels away, or removes from its underlying layer of support tissue at the back of the eye. The retina is a thin layer of light-sensitive afferent neuron at the back of the eye. We require a healthy retina to be able to see plainly.
In the beginning, detachment might just take place in a small part of the retina, however, without proper treatment, the entire retina might remove, and vision will be lost from that eye.
In most cases, detached retina, or retinal detachment, only happens in one eye. It is a medical emergency situation.
People with severe myopia, those with diabetes, patients who have had complicated cataract surgery, and anyone who has actually received a blow to the eye are all more vulnerable to the condition.
What Is Retinal Detachment?
Light goes through the optical system of the eye and strikes the retina, like in a nondigital cam.
The image produced by the light that hits the retina is translated into neural impulses and sent to the brain through the optic nerve.
Simply puts, an image focuses on the retina, afferent neuron process the info, and they send it by electrical impulses through the optic nerve to the brain.
There are three types of detached retina:
- Rhegmatogenous retinal detachment is a break, tear, or hole in the retina. This hole enables liquid to pass from the vitreous space into the subretinal space in between the sensory retina and the retinal pigment epithelium. The pigment epithelium is the pigmented cell layer just outside the neurosensory retina.
- Secondary retinal detachment is likewise called exudative retinal detachment or serous retinal detachment. It takes place when swelling, vascular irregularities, or injury cause fluid to develop under the retina. There is no hole, break, or tear.
- Tractional retinal detachment is when an injury, inflammation, or neovascularization causes the fibrovascular tissue to pull the sensory retina from the retinal pigment epithelium.
Symptoms and Signs of Detached Retina
An individual with a detached retina might experience a number of symptoms.
These consist of:
- Photopsia, or sudden, brief flashes of light outside the central part of their vision, or peripheral vision. The flashes are most likely to take place when the eye relocations.
- A significant boost in the number of floaters, the littles debris in the eye that make us see things floating in front of us, usually like little strings of transparent bubbles or rods that follow our visual field as our eyes turn. They might see what looks like a ring of hairs or floaters on the peripheral side of the vision.
- A heavy sensation in the eye
- A shadow that begins to appear in the peripheral vision and slowly spreads to the center of the field of view
- A sensation that a transparent curtain is coming down over the visual field
- Straight lines start to appear curved
It is not generally painful.
What Causes Retinal Detachment?
The retina is the layer of tissue that lines the inside of the eye. It is light sensitive and its function is to send visual signals to the brain, through the optic nerve.
Retinal detachment happens when this layer is pulled from its normal position. In some cases, there are small tears in the retina. These, too, can cause the retina to become detached.
Factors that may increase the risk of developing retinal detachment include:
- Genetics, for instance, if a close family relative has actually had retinal detachment
- Middle and older age
- Severe nearsightedness
- Previous cataract surgery, particularly if it was complicated
- Previous retinal detachment
- Eye conditions, such as uveitis, degenerative myopia, lattice degeneration, and retinoschisis
- Trauma, for instance, a blow to the eye
- Diabetes, particularly if the diabetes is poorly managed
Anybody with these risk factors must know the possibility of a detached retina.
Treatment Options for Detached Retina
If a doctor suspects retinal detachment, they will generally refer the patient to an eye specialist, or ophthalmologist, for an exact diagnosis.
The eye doctor will examine they eye after dilating, or widening, the students with eye drops. An ultrasound might provide more detail.
Surgery will be required to discover all the retinal breaks and seal them and to alleviate present and future vitreoretinal traction, or pulling. Without surgery, there is a high risk of total vision loss.
Alternatives for surgery include:
- Laser surgery, or photocoagulation: A laser beam is directed through a contact lens or ophthalmoscope. The laser burns around the retinal tear, leading to scarring tissue that then merges the tissue back together.
- Cryotherapy: Cryosurgery, cryopexy, or freezing, includes applying severe cold to destroy unusual or infected tissue. The procedure produces a delicate scar that helps connect the retina to the wall of the eye.
- Scleral buckling: In the area where the retina has actually detached, really thin bands of silicone rubber or sponge are stitched onto the sclera, the outdoors white of the eye. The tissue around the area might be frozen or lasers may be used to scar the tissue.
- Vitrectomy: The vitreous gel is removed from the eye and a gas bubble or silicon oil bubble is used to hold the retina in place. The wound is sewn. Silicon oil has to be removed 2 to 8 months after the procedure.
- Pneumatic retinopexy: This can be used if the detachment is straightforward. The surgeon freezes the tear area, using cryopexy, before injecting a bubble into the vitreous cavity of the eye. This pushes the retina back against the tear and the detached area, preventing additional circulation of fluid behind the retina. After some days, the pressure eventually makes the retina reattach itself to the wall of the back of the eye.
A person who has a gas bubble positioned in the eye may be encouraged to hold the head in a particular way for some time, and they will not be allowed to fly. If an oil bubble is used, flying is enabled.
Researchers have actually been looking into the use of silicone oil to treat proliferative vitreoretinopathy (PVR), a problem of retinal detachment surgery that can cause more detachment of the retina.
The National Eye Institute quote that around 90 percent of treatments for retinal detachment are successful, although some people will need further treatment.
Often, it is not possible to reattach the retina, and the individual’s vision will continue to deteriorate.
The patient’s vision must return a couple of weeks after treatment. If the macula is involved in the detachment, the individual’s sight may never ever be as clear as it was previously. The macula is the part of the eye that enables us to see what is straight in front of us.
The cost of surgery for retinal detachment depends on the kind of procedure. Research published in 2014 recommends that “treatment and prevention of RD are incredibly cost reliable compared with other treatment of other retinal disease, no matter treatment modality.”
The research study, released in the journal Ophthalomology, stabilized the cost of treatment against the advantages of good eyesight and lifestyle.
There is a little risk of complications after surgery. These include allergic reactions to medications, bleeding in the eye, double vision, cataracts, glaucoma, and eye infection.
Participating in regular vision tests can help to minimize the risk of retinal detachment, as eye conditions such as this can often be identified in the early stages.