In wet (neovascular/exudative) age-related macular degeneration (AMD), unusual capillary develop under the macula and break, bleed, and leak fluid. This damages the macula and, if left neglected, can lead to quick and severe loss of main vision. The most efficient treatments to date for wet AMD are numerous anti-angiogenic drugs.
Angiogenesis is a term used to explain the growth of new members vessels and plays an essential function in the normal development of body organs and tissue. Often, nevertheless, excessive and abnormal blood vessel advancement can occur in diseases such as cancer (tumor growth) and AMD (retinal and macular bleeding).
Substances that stop the development of these excessive capillary are called anti-angiogenic (anti = against; angio = vessel; genic = development), and anti-neovascular (anti = versus; neo = brand-new; vascular = capillary).
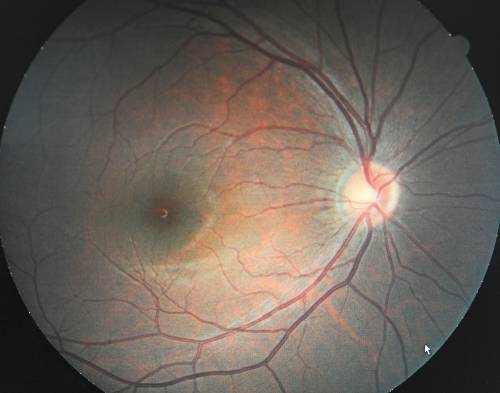
The focus of current anti-angiogenic drug treatments for wet AMD is to reduce the level of a particular protein called vascular endothelial development factor, or VEGF, that promotes abnormal blood vessel growth in the retina and macula; therefore, these drugs are categorized as anti-VEGF treatments.
Treating Wet Macular Degeneration with Medicines
At present, these drugs are administered by injection directly into the eye after the surface has been numbed. The needle is extremely little and is placed near the corner of the eye– not the center. During the injection procedure, the doctor will ask the patient to search in the opposite direction to expose the injection site, which likewise allows the patient to prevent seeing the needle. Anti-angiogenic drugs presently in use consist of Lucentis, Avastin, and Eylea. An earlier drug, Macugen, is also used in particular situations.
Medical Trials for Wet Macular Degeneration
In order to receive approval from the U.S. Food and Drug Administration (FDA), a new drug or treatment need to be proven to be both safe and efficient by going through a rigorous series of regulated objective studies. To avoid bias, neither the patient nor the inspectors can understand which patients received the real treatment and which were the without treatment (or “control”) subjects.
These are called “double blind” or “double masked” research studies and typically yield the most reputable results. The medication is coded and patients are positioned at random into either the treatment or control group. When the study is concluded, the code is exposed and it is then possible to determine who received the real drug and who received the non-active substance, or placebo.
As defined by the U.S. National Institutes of Health, most scientific trials are designated as Phase I, II, or III, based on the concerns the research study is looking for to respond to:
- In Phase I medical trials, scientists test a new drug or treatment in a little group of people (20-80) for the first time to evaluate its safety, determine a safe and effective dose range, and recognize possible side effects.
- In Phase II clinical trials, the research study drug or treatment is provided to a larger group of people (100-300) to determine if it works and to additional evaluate its safety.
- In Phase III research studies, the research study drug or treatment is provided to even bigger groups of people (1,000-3,000) to validate its efficiency, screen side effects, compare it to commonly used treatments, and gather information that will permit the drug or treatment to be used securely.
- In Phase IV research studies, after the Food and Drug Administration has approved the drug, continuing studies will figure out extra info, such as the drug’s risks, side effects, benefits, and optimal use.
Other Treatments for Wet AMD
Photodynamic Therapy
Photodynamic therapy (PDT) was established by scientists at the Massachusetts Eye and Ear Infirmary and has actually been authorized for AMD treatment by the FDA given that April 2000. PDT works as follows: A 10-minute intravenous administration of Visudyne (a light-sensitive drug) is followed by the application of a low-dose, non-thermal (light just) laser to the affected area of the retina. The drug flows throughout the body’s blood vessels, and is particularly drawn in to new members vessels, including the abnormal vessels under the macula.
The laser activates the drug, which selectively seals off the leaking capillary without harming the surrounding healthy retinal tissue. This function permits PDT to be used straight underneath the center of the macula, unlike thermal (heat) laser photocoagulation, which can burn and ruin normal retinal tissue.
Thermal Laser Photocoagulation
Thermal laser photocoagulation is a strategy used by retinal surgeons to treat a number of eye conditions, among which is wet AMD. A thermal (heat) laser is directed into the eye at irregular capillary growing beneath the retina. The heat from the laser blocks the undesirable blood vessels, avoiding additional leakage and vision loss.
Thermal laser photocoagulation does not restore lost vision; therefore, in the past, it was crucial that treatment be initiated as early as possible in the course of the disease. Unlike PDT, however, thermal laser can likewise ruin surrounding healthy retinal tissue as it seals the leak from irregular blood vessel development; therefore, it is not used on vessels directly under the center of the macula. At present, thermal laser is seldom used in scientific practice.
Macular Translocation Surgery
Macular translocation is a surgery that includes detaching the retina from its base, rotating it a little, and changing it in a different position, so that the macula rests on a brand-new, healthy base. While macular translocation surgery is unlikely to become basic treatment for everyone with wet AMD, it has proven reliable for some people when done immediately. It does not work for dry AMD since, for reasons not yet comprehended, the degeneration repeats in the new position.
Have an Eye Examination
If you have actually not had an eye exam by an eye doctor in 3 or more years, you may get approved for aid from the AMD Eye Care Program, offered through the American Academy of Ophthalmology. The program provides complimentary eye tests for individuals who have not been identified with AMD, are age 65 and older, are U.S. citizens or legal citizens, and do not belong to an HMO or the Veterans’ Administration (VA).