Imagine waking up one day and realizing your side vision is fading—as if the world has slowly started closing in. That’s tunnel vision. It doesn’t mean you’re going blind tomorrow, but it does mean your eyes are asking for help. This kind of vision loss often starts so quietly, many people don’t even know it’s happening until it interferes with everyday life.
Prevalence of Vision Loss by Age in the U.S.
| Age Group | Vision Loss (%) |
|---|---|
| 0–17 | 1.16% |
| 18–39 | ~1.4% |
| 40–64 | ~3.5% |
| 65–84 | ~6.5% |
| 85+ | ~10% |
This chart shows how common vision impairment (defined as 20/40 vision or worse) is across different age groups in the U.S. Prevalence increases notably with age, peaking among adults over 85, emphasizing the need for age-targeted vision care strategies.
The good news? We now have more tools than ever to catch it early, understand its causes, and slow or manage its progression. This guide walks you through what to expect—and how to stay one step ahead.

What Causes Tunnel Vision?
Tunnel vision isn’t a disease itself—it’s a symptom of deeper issues, like the warning light on a car dashboard. The root causes vary, but they all share one thing in common: they interfere with the way your eyes or brain receive and process visual information from the sides. Let’s break it down.
- Glaucoma: Think of your eye as a balloon with fluid inside. In glaucoma, the pressure builds up too high, slowly crushing the optic nerve that sends signals to the brain. This nerve damage starts at the edges of your vision—meaning you might not notice it until it’s advanced.
- Retinitis Pigmentosa (RP): This genetic condition is like a slow dimming of the lights in your peripheral vision. Specialized cells in your retina (rods) gradually stop working. It often begins with night blindness and then narrows the field of vision over time. People with RP may feel like they’re looking through a tunnel by their 30s or 40s ⧉.
- Stroke or Brain Injury: The brain processes vision in its occipital lobe at the back of the head. When a stroke or trauma affects this region, the brain might not interpret visual data from one or both sides, resulting in a narrowed field of view. It’s not the eyes—it’s the signal processing that’s impaired.
- Diabetic Retinopathy: Diabetes affects small blood vessels, including those in your retina. Imagine trying to look through a fogged-up window—the blood leakage and swelling obscure your vision. Over time, if untreated, it can contribute to tunnel vision due to peripheral retinal damage ⧉.
- Optic Neuritis: Often linked to multiple sclerosis (MS), this is inflammation of the optic nerve. When inflamed, the nerve doesn’t transmit visual signals effectively. People may experience pain and vision loss, often in one eye. Recovery is possible, but repeated episodes can reduce the visual field permanently.
Understanding these causes is key—not only to treating tunnel vision early but to preventing it altogether. If your family has a history of eye conditions, or you’re managing chronic illness like diabetes, this section should be a wake-up call.
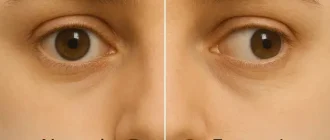
Tunnel Vision Snapshot
How Is It Diagnosed?
Diagnosing tunnel vision involves a battery of tests that evaluate the extent and cause of vision loss. Here’s a closer look:
Visual Field Test (Perimetry)
- How it works: The patient sits facing a large, dome-shaped machine and is instructed to focus on a central dot. Tiny lights will flash randomly in the peripheral areas, and the patient presses a button each time they see one. It’s a bit like playing a reaction game in slow motion. The machine maps what areas of the visual field respond. The test is painless and typically takes 15–30 minutes.
- Accuracy: 9/10 for detecting early peripheral vision loss.
- Cost: $150–$250 (approx. €140–€230) in the U.S. ⧉
Optical Coherence Tomography (OCT)
- How it works: This test involves sitting in front of a small machine where you place your chin and forehead on supports. A light beam scans your retina without touching the eye, creating detailed cross-section images. It’s similar to getting an ultrasound—except with light, not sound. The whole procedure takes under 10 minutes, and results are available almost immediately.
- Accuracy: 8.5/10 for structural analysis.
- Cost: $100–$200 (€95–€190).
Fundus Photography
- How it works: A high-resolution camera is used to capture images of the back of the eye. You’ll likely be given eye drops to dilate your pupils beforehand, which might cause slight blurriness for a few hours. The process itself is as simple as having your photo taken—with a very bright flash. The images help detect abnormalities in the retina and optic nerve.
- Accuracy: 7.5/10.
- Cost: $75–$150 (€70–€140).
Case Example: Real-Life Tunnel Vision Story
A 47-year-old male from Austin, Texas, experienced repeated minor car accidents. Initially attributing them to stress, he eventually saw an ophthalmologist who diagnosed advanced glaucoma. Despite therapy, his field of vision had already narrowed to a 10-degree central circle—highlighting the need for early detection.
Tunnel Vision Risk—Vision Conditions Contribution
| Condition | Estimated U.S. Cases |
|---|---|
| Retinitis Pigmentosa (RP) | ~100,000 |
| Stroke (Hemianopia) | ~800,000 |
| Glaucoma | 1.49 million |
| Diabetic Retinopathy | ~9.6 million* |
This chart compares the estimated number of Americans affected by conditions contributing to tunnel vision. While retinitis pigmentosa is rare, diabetic retinopathy and glaucoma are major contributors, with stroke also playing a notable role. *Only a portion of diabetic retinopathy cases lead to peripheral field loss.
Treatment Options for Tunnel Vision
Tunnel vision itself—defined as the loss of peripheral visual fields—is rarely reversible. However, there are medical, surgical, and technological interventions designed to treat its causes and improve a patient’s quality of life. Here’s a breakdown of current approaches in the U.S. healthcare system:
Addressing Underlying Causes
When tunnel vision stems from glaucoma, diabetic retinopathy, or optic neuritis, treatment is focused on stopping further damage.
Glaucoma Treatment
- Medications: First-line options include prostaglandin analogs like latanoprost (Xalatan®), beta-blockers (timolol), and carbonic anhydrase inhibitors (dorzolamide).
- Surgical Options: Trabeculectomy and laser therapies (like SLT—Selective Laser Trabeculoplasty).
- Effectiveness: High for pressure control (8–9/10), but limited for vision recovery.
- Costs: Eye drops range $30–$100/month without insurance; surgeries $1,000–$3,000 per eye.
- Patient Journey: Regular pressure checks, long-term medication adherence, potential outpatient procedures.
Diabetic Retinopathy Treatment
- Injections: Anti-VEGF drugs (Lucentis®, Eylea®) help reduce blood vessel overgrowth.
- Laser Treatment: Panretinal photocoagulation to seal leaking vessels.
- Effectiveness: Moderate (6–8/10) for vision stabilization.
- Costs: Injections cost $1,500–$2,000 per dose; laser therapy ~$500–$1,200/session.
- Experience: Injections are done in-office with topical anesthesia; multiple treatments needed.
Optic Neuritis Treatment
- Medication: High-dose intravenous corticosteroids like methylprednisolone, followed by oral taper.
- Associated Care: Often managed alongside neurologists if MS is involved.
- Effectiveness: Vision improves in 90% of cases within weeks.
- Costs: $1,000–$3,000 per course.
Neuroprotective Therapies
Experimental in nature, these are aimed at preserving optic nerve function.
- Agents: Brimonidine tartrate (also lowers pressure), citicoline supplements.
- Effectiveness: Still under investigation (rated 5/10).
- Availability: Limited to clinical trials or off-label use.
Gene Therapy
Best suited for inherited conditions like retinitis pigmentosa.
- Treatment: Clinical trials with gene replacement or editing (e.g., Luxturna® for RPE65 mutation).
- Delivery: Subretinal injection under general anesthesia.
- Effectiveness: Early trials show promising stabilization or mild improvements.
- Cost: Extremely high—Luxturna® costs ~$850,000 total.
Retinal Prosthetics
Technologies designed to bypass damaged photoreceptors.
- Example: Argus II® Retinal Prosthesis System ⧉
- How It Works: A tiny camera mounted on glasses sends signals to a retinal implant.
- Effectiveness: Allows basic object recognition and movement detection (rated 6/10).
- Cost: Up to $150,000 including surgery.
Rehabilitation and Compensation
When peripheral vision cannot be restored, occupational therapy steps in.
- Tools: Field-enhancing lenses (like Peli lenses), screen readers, magnifying tablets.
- Training: Orientation and mobility specialists teach scanning strategies.
- Effectiveness: High for quality-of-life improvement.
- Support: Usually covered under low vision rehabilitation services.
How to Adapt to Living with Tunnel Vision
- Use visual aids: Special prism glasses expand perceived visual field.
- Home adjustments: Remove clutter, install brighter lighting.
- Mobility training: Orientation and mobility specialists teach safe navigation.
Useful Table: Peripheral Vision Conditions vs. Treatment
| Condition | Key Feature | Primary Treatment | Reversibility |
|---|---|---|---|
| Glaucoma | High IOP, optic nerve | Drops, laser, surgery | No |
| Retinitis Pigmentosa | Genetic, night blindness | Vitamin A, gene therapy (future) | No |
| Diabetic Retinopathy | Vascular damage | Anti-VEGF, laser | Partially |
| Optic Neuritis | Inflammation | Steroids, MS management | Partially |
Editorial Advice
Tunnel vision isn’t just a visual condition—it’s a lifestyle disruptor. Reyus Mammadli, medical consultant, recommends early and regular screening, especially for those with risk factors like diabetes or a family history of glaucoma. “Most cases don’t scream for attention until it’s too late,” he notes. “If you’re bumping into things more often, it’s time to get checked.”
Additional tips:
- Annual eye exams for individuals over 40.
- Discuss genetic testing if there’s a family history.
- Ask about the latest clinical trials for emerging therapies ⧉.
Being proactive is more than a buzzword—it’s your best line of defense against peripheral vision loss.
Glaucoma Prevalence by Race (U.S.)
| Race/Ethnicity | Prevalence (%) |
|---|---|
| White | 1.42% |
| Hispanic & Other | 1.56% |
| Black | 3.15% |
This chart highlights racial disparities in glaucoma prevalence in the U.S. Black Americans show the highest rates, more than double those of White individuals, underscoring the importance of targeted public health interventions and early screening in high-risk populations.