Blurry vision in the morning might seem like one of those “wake-up quirks,” but it often signals something more specific going on with your eyes—or your overall health. During sleep, your eyes are closed for several hours, which naturally affects moisture levels, pressure, and tear film quality. When you first open your eyes, the world might appear fuzzy, hazy, or smeared, like trying to look through a fogged-up windshield.
Source: eyexan.com
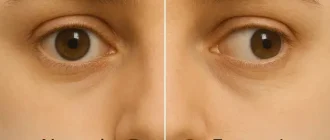
One common culprit is dry eye syndrome, where the tear glands don’t produce enough lubrication overnight. This condition is especially prevalent in individuals over 50, but younger adults glued to screens all day aren’t off the hook either. Sleeping with a fan, AC, or in low humidity environments can make it worse ⧉.
Another reason? Eye discharge—yep, that “sleep crust”—which can temporarily blur your vision until it’s cleared. Swelling of the cornea or eyelids (often related to allergies or poor sleeping posture) may also play a part. And don’t overlook nocturnal lagophthalmos, a condition where the eyelids don’t fully close during sleep, causing exposure-related dryness.
Morning Blurry Vision Causes Breakdown
The chart illustrates common reasons behind waking up with blurred vision, with dry eye syndrome being the most frequent cause. Based on data from Healthline and the Sleep Foundation, the visualization emphasizes the relative frequency of each condition that contributes to morning blur.
Could It Be a Sign of Something More Serious?
In some cases, morning blurry vision is more than a nuisance—it can be a red flag. For instance, a sudden, one-eye-only blur might signal optic neuritis, often associated with multiple sclerosis, or a warning sign of a transient ischemic attack (mini-stroke). Both situations require immediate attention.
People with diabetes may experience blurry vision in the morning due to fluctuating blood sugar levels affecting the shape of the lens inside the eye ⧉. Similarly, high blood pressure can lead to fluid buildup under the retina (central serous retinopathy), which tends to cause visual distortion right after waking.
Percentage Who Experience Morning Blur Regularly
This chart shows how often people wake up with blurred vision. While a smaller group experiences it daily, the majority report it occasionally or several times a week. The distribution is based on insights from Healthline, which notes that morning blur “happens to a lot of people.”
Glaucoma, particularly normal-tension glaucoma, can quietly damage the optic nerve overnight. Since intraocular pressure naturally spikes in the early morning, individuals at risk may notice subtle vision changes at that time ⧉.
Diagnostic Tools and Accuracy
A proper diagnosis begins with a comprehensive eye exam, which typically includes:
- Slit-lamp examination: This is a close-up look at your eye under a special microscope combined with a bright light. You sit in a chair with your chin on a support while the doctor moves the slit lamp in front of your face to inspect your tear film, cornea, and other front structures of the eye. Accuracy: 9/10.
Cost: $80–$200. - Optical Coherence Tomography (OCT): Think of this as an “MRI for your eyes.” While seated, you look into a lens and stay still as the machine scans your retina and optic nerve with light waves—no contact, no pain. It reveals layers of the retina in cross-section, helping detect swelling, fluid, or nerve damage. Accuracy: 9.5/10.
Cost: $100–$300. - Tonometry: This test measures the pressure inside your eyes (intraocular pressure). There are a few types, but the most common involves a puff of air directed at your eye or a gentle device that briefly touches the surface. You rest your chin and forehead on a support as it’s done. Accuracy: 8/10.
Cost: $60–$100. - Tear breakup time test: This evaluates how long your tear film stays stable after a blink. The eye doctor places a small amount of dye (fluorescein) into your eye and views it under blue light to see how quickly the tears evaporate. The test is simple, quick, and helps diagnose dry eye syndrome. Accuracy: 8/10.
Cost: Often included in regular exams.
Reyus Mammadli, medical consultant, recommends not skipping your annual eye exams—even if symptoms seem minor: “Morning blur might feel like no big deal, but it can be the earliest signal of chronic issues.”
Real People, Real Mornings: Blurry Vision Stories
One man in his mid-30s from Colorado shared how his mornings began with what he called “shower-glass vision”—blurry, misty, and disorienting. He ignored it for months, thinking it was just due to poor sleep. After visiting a doctor, he was diagnosed with meibomian gland dysfunction. With thermal therapy and a daily lid-cleaning routine, his mornings finally cleared up.
A retiree from Florida, aged 68, noticed that her right eye was always foggy for 15–20 minutes after waking. She feared the worst, but it turned out to be related to poorly controlled dry eye syndrome. Her ophthalmologist recommended preservative-free drops and a humidifier at night. Within weeks, she reported “waking up to clarity” most days.
Another case involved a young woman, 27, working long hours in tech. She thought her blurry mornings were just screen fatigue catching up with her. But a routine eye exam revealed elevated intraocular pressure—an early sign of glaucoma. Now, with nightly drops and follow-ups, her vision is stable, and she’s thankful she caught it in time.
Each of these stories starts with morning blur—but none ends in defeat. With attention and the right treatment, clarity often returns. Many Americans are caught off guard when something they dismissed as “just tired eyes” turns out to be a silent chronic condition ⧉.
How to Treat Morning Blurry Vision
Dry Eyes
Dry eye syndrome occurs when the eyes don’t produce enough quality tears for lubrication, especially overnight. It often results in stinging, burning, and blurred vision upon waking.
Treatment: Use preservative-free lubricating eye drops such as Systane Ultra or Refresh Optive, typically 1–2 drops in each eye, 3–4 times daily. For more advanced cases, ophthalmologists may recommend punctal plugs to block tear drainage or prescription eye drops like cyclosporine (Restasis), used twice daily.
Effectiveness: 8.5/10.
Cost: $15–$30/month for OTC drops; up to $600 for Restasis per month; punctal plug procedure: $300–$500 (one-time).
Allergic Swelling
Allergic conjunctivitis leads to inflammation in the eyelids and conjunctiva, often causing puffiness and blurred vision after sleep.
Treatment: Over-the-counter antihistamine drops like Zaditor (ketotifen) or prescription-strength olopatadine (Pataday). Drops are usually applied once or twice daily. Cold compresses and allergen avoidance (like removing pets from the bedroom) also help.
Effectiveness: 8/10.
Cost: $15–$40/month for OTC; $100–$150/month for prescription drops.
Poor Sleep Posture
Sleeping face-down or with pressure on one side of the face can compress the eye and disrupt tear distribution, leading to temporary blur.
Treatment: Use a contoured memory foam pillow or back-sleeping wedge to relieve pressure on the eyes. No medical procedures are necessary unless posture contributes to lid dysfunction or nocturnal lagophthalmos.
Effectiveness: 7.5/10.
Cost: $30–$80 for ergonomic pillows.
Underlying Conditions (e.g., Glaucoma)
Glaucoma causes progressive damage to the optic nerve, sometimes exacerbated by early-morning intraocular pressure spikes.
Treatment: Prostaglandin analogs like latanoprost (Xalatan) or bimatoprost (Lumigan) reduce eye pressure. These are usually applied as eye drops once daily at night. In some cases, laser therapy (e.g., selective laser trabeculoplasty) is used.
Effectiveness: 9/10.
Cost: $25–$70/month for medications; $500–$1,500 for laser procedures.
Meibomian Gland Dysfunction (MGD)
MGD affects oil glands along the eyelids, leading to evaporative dry eye and blur, particularly in the morning.
Treatment: In-office thermal pulsation therapy (e.g., LipiFlow) warms and massages the glands to restore oil flow. Usually done once or twice a year. Patients may also be prescribed doxycycline (oral, low dose) for inflammation.
Effectiveness: 8.5/10.
Cost: $700–$1,000 per session; $30–$50/month for doxycycline.
Chronic Dry Eye (Advanced)
In patients with persistent symptoms, including postmenopausal women or long-term contact lens wearers, chronic dry eye may be resistant to drops alone.
Treatment: Intense Pulsed Light (IPL) therapy improves tear stability and reduces inflammation. Sessions last 15–20 minutes, typically done in 3–4 rounds, spaced weeks apart.
Effectiveness: 9/10.
Cost: $400–$600 per session (usually not covered by insurance).
Innovative options include thermal pulsation therapy for meibomian gland dysfunction and intense pulsed light therapy (IPL), which has shown promise for chronic dry eye sufferers ⧉.
Prevention Tips You Can Actually Use
- Blink more often during screen time. Sounds basic, but it works. Set a reminder to blink every 20 seconds when working on a computer—it keeps the tear film stable and prevents your eyes from drying out.
- Hydrate well—especially before bed. Dehydration reduces tear production, making eyes more vulnerable in the morning. Drink a full glass of water an hour before sleep to support overnight eye health.
- Avoid caffeine close to bedtime; it can interfere with tear production. Try cutting off caffeine by 2–3 p.m. to avoid drying out your eyes overnight. Swap late-day coffee for herbal tea to stay hydrated without affecting sleep.
- Don’t ignore your eyelids—clean them with lid scrubs to reduce bacterial buildup. Use pre-moistened eyelid wipes or a warm compress every evening. This helps unclog meibomian glands and improves morning comfort.
- Use blue light filters on devices to minimize eye strain that can carry over into the morning. Activate “night mode” or install apps like f.lux that reduce screen glare. Your eyes will feel less fatigued by morning, and you’ll sleep better too.
Blur Resolution Time After Waking
This chart shows how long it typically takes for morning blurriness to clear on its own. The majority of people report that blinking resolves it in under a minute, while others may experience residual blur for up to 15 minutes. Data is based on Healthline descriptions of temporary vs. prolonged morning blur.
Editorial Advice
If your vision seems foggy every morning, don’t wait for it to become your “new normal.” As Reyus Mammadli emphasizes, “Vision is one of the senses we tend to take for granted—until clarity is lost.”
Many early interventions are simple and noninvasive. But the first step is always the same: listen to your body (and your eyes), and seek medical advice sooner rather than later. After all, the world looks a whole lot better when it’s in focus.