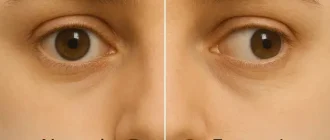
Dry eye syndrome, also known as keratoconjunctivitis sicca, is more than just a temporary discomfort. It occurs when your eyes either don’t produce enough tears or produce poor-quality tears that evaporate too quickly. The result? Your eyes can’t stay lubricated the way they should.
Who’s Most at Risk for Dry Eyes?
Age and gender significantly impact the risk of developing chronic dry eye disease. Here’s what the stats reveal.
🎯 Women over 50 are almost twice as likely to develop chronic dry eyes. Age and hormones play a major role in tear film imbalance.
Source: eyexan.com
According to the American Academy of Ophthalmology ⧉, over 16 million Americans are officially diagnosed with dry eye disease, and many more go undiagnosed. Women over 50 are particularly prone to it, especially post-menopause. But let’s be honest — in our digital world, age isn’t the only factor. Screen time is doing a number on our blink rate, which leads to increased dryness.
Reyus Mammadli, medical consultant, emphasizes, “Dry eye isn’t just about feeling uncomfortable. It can alter your vision significantly if left untreated.”
So… Can Dry Eyes Really Mess with Your Vision?
Yes — and not in a subtle way. Dry eyes can cause fluctuating vision, meaning your eyesight may be clear one moment and blurry the next. That’s because your tear film — the thin layer of moisture covering your eye — is essential for sharp vision. Without it, light doesn’t refract correctly.
Some common visual disturbances associated with dry eyes include:
- Blurred vision
This is one of the clearest and most frequent indicators of dry eye. It usually appears as a hazy or fluctuating blur that improves temporarily after blinking or applying eye drops — a strong sign your tear film isn’t stable. - Double vision (diplopia)
Less common but more concerning, this symptom may appear intermittently when the eye surface is highly irregular. If it disappears after rest or eye lubrication, dry eye could be the underlying issue. - Eye fatigue
A very common symptom in the digital age. On its own, it’s not diagnostic — but when paired with dryness, burning, or gritty sensations, it strongly supports a dry eye diagnosis. - Sensitivity to light
Also called photophobia, this symptom becomes more noticeable in dry eye patients during prolonged screen use or outdoor exposure. It’s often linked to surface irritation and inflammation. - Difficulty driving at night
This is a particularly telling sign of dry eye disrupting vision. People often report halos around lights, glare, and trouble with contrast in low-light conditions — classic effects of an unstable tear film.
In a clinical study by the National Eye Institute ⧉, participants with dry eyes were found to have significantly reduced contrast sensitivity, a key component of clear, comfortable vision.
And here’s the kicker: some patients even report feeling like there’s a film or haze over their eyes. Spoiler alert — it’s not your glasses.
What’s Behind the Blur? The Science of Dry Eyes and Vision Distortion
The cornea — your eye’s front surface — relies on the tear film to maintain a smooth, refractive surface. When tears are unstable or evaporate too quickly, the cornea dries out, disrupting the way light is focused onto the retina. This leads to visual distortion.
According to a 2024 article published in Ophthalmology Times ⧉, even minor inconsistencies in tear quality can lower visual acuity by up to 25% in chronic cases.
It gets worse if you wear contact lenses. The lens can exacerbate dryness, leading to even more irritation and visual disturbances. In some cases, this creates a vicious cycle — dry eyes cause blurry vision, which causes squinting, which worsens the dryness. Fun, right?
How Screen Time Impacts Dry Eye Risk
Spending long hours staring at screens can dramatically increase your chances of developing dry eye symptoms.
This means over one-third of moderate screen users already show symptoms — especially office workers and students.
High screen time dries the eyes faster by reducing blinking rate and increasing tear film evaporation.
Lower screen exposure gives your eyes more natural breaks and blink rhythm, protecting the tear layer.
💡 Tip: Follow the 20–20–20 rule. Every 20 minutes, look at something 20 feet away for 20 seconds to reduce digital eye strain.
Source: eyexan.com
Diagnosis: How Doctors Detect Dry Eye-Related Vision Issues
Diagnosing dry eyes goes beyond a quick glance.
Here are the most commonly used tools:
1. Schirmer’s Test
- How it works: Small strips of paper are placed under the eyelid to measure tear production.
- Self-experience: It can feel slightly ticklish or irritating for a few minutes, but it’s not painful. You’ll sit with your eyes closed for about 5 minutes as the paper absorbs tears.
- Accuracy: 7/10
- Average Cost: $75–$150
2. Tear Break-Up Time (TBUT)
- How it works: A dye is placed in the eye and observed under blue light to see how quickly tears evaporate.
- Self-experience: You’ll get a drop in the eye, then look straight ahead without blinking. The doctor uses a special lamp to watch how fast the tear film breaks apart.
- Accuracy: 8/10
- Average Cost: $50–$100
3. LipiView and Meibography
- How it works: Advanced imaging that visualizes oil glands and tear film structure.
- Self-experience: You rest your chin in a scanner while it takes high-res pictures. Totally painless and takes just a couple of minutes.
- Accuracy: 9/10
- Average Cost: $200–$350
4. InflammaDry Test
- How it works: Detects MMP-9, an inflammatory marker found in dry eye patients ⧉.
- Self-experience: A soft swab gently touches the inside of your lower eyelid — it’s quick and feels like a Q-tip swipe.
- Accuracy: 8.5/10
- Average Cost: $100–$200
In a memorable case, a 38-year-old software engineer from Austin, TX, reported severe visual fluctuations during coding sessions. His LipiView imaging showed meibomian gland dysfunction — a common culprit in evaporative dry eye. After treatment, his vision stabilized, and his productivity soared.
Modern Treatments: Beyond Artificial Tears

While over-the-counter lubricating drops are the go-to, they’re not the be-all-end-all. The treatment landscape has grown impressively sophisticated.
Prescription Medications
- Restasis (cyclosporine) and Xiidra (lifitegrast) reduce inflammation and boost tear production.
- Tyrvaya nasal spray is a newcomer that stimulates natural tear production via the trigeminal nerve ⧉.
In-Office Procedures
- LipiFlow: Heat and massage to unblock meibomian glands.
- IPL (Intense Pulsed Light): Targets inflammation around the eyelids.
- Punctal Plugs: Tiny devices that block tear drainage, keeping the eye moist longer.
Cutting-Edge Tech
According to the American Optometric Association ⧉, innovations like iLux and TrueTear are redefining dry eye care with impressive patient satisfaction rates.
Reyus Mammadli advises, “If your vision fluctuates or worsens by the end of the day, it’s not just fatigue. Get checked for dry eye disease — modern treatments are game-changers.”
Prevention Tips That Actually Work
Sometimes it’s the little things that save your sight:
- Follow the 20-20-20 Rule: Every 20 minutes, look at something 20 feet (6 meters) away for 20 seconds.
- Hydrate like it’s your job. Dehydration makes dryness worse.
- Blink, blink, blink. Especially during screen use.
- Use a humidifier — it’s a game-changer during winter.
- Omega-3s (via diet or supplements) may improve tear quality ⧉.
Even simple tricks like warm compresses or lid hygiene can go a long way.
Editorial Advice
If your eyes feel gritty, your vision is hazy, or your contact lenses seem cursed by a vengeful optometrist, it might be time to consider dry eyes as the culprit.
Reyus Mammadli, medical consultant, recommends addressing symptoms early: “Chronic dry eye can sneak up on you. Even mild symptoms, if ignored, may evolve into persistent visual problems.”
Don’t wait for the world to get blurry. If you experience recurring visual fluctuations or eye discomfort, see an eye care professional. The longer you wait, the harder it is to treat. Prevention is easier, treatment is better, and frankly — your eyes deserve it.
Types of Dry Eye & What Triggers Them
Dry eye isn’t just one condition. There are two main types, each with different causes and treatment priorities.
Aqueous-Deficient Dry Eye
Caused by reduced tear production, often linked to aging, autoimmune diseases (like Sjögren’s), or certain medications.
🧴 You may feel constant dryness even in calm environments — artificial tears help but don’t last long.
Evaporative Dry Eye
Happens when your tears evaporate too fast due to blocked oil glands, screen overuse, or environmental conditions.
🟡 Your eyes may water excessively but still feel dry or gritty — warmth and gland treatments often help.
Mixed-Type Dry Eye
A combination of both types — the most common form. Especially seen in older adults and people with multiple risk factors.
⚠️ If no drops seem to work and symptoms vary, you likely have a mixed case needing full evaluation.
🔎 Understanding your dry eye type helps target treatment. Don’t just use random drops — match the fix to the cause.
Source: eyexan.com