Phacoemulsification is a modern cataract surgery where the eye’s internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are changed with irrigation of balanced salt solution to keep the anterior chamber.
What Is Phacoemulsification?
The term originated from phaco- (Greek phako-, comb. form of phakós, lentil; see lens) + emulsification.
Preparation and preventative measures
Proper anesthesia is essential for ocular surgery. Topical anesthesia is most commonly employed, typically by the instillation of a local anesthetic such as tetracaine or lidocaine. Additionally, lidocaine and/or longer-acting bupivacaine anesthestic might be injected into the area surrounding (peribulbar block) or behind (retrobulbar block) the eye muscle cone to more totally incapacitate the extraocular muscles and reduce pain experience. A facial nerve block using lidocaine and bupivacaine might sometimes be performed to minimize cover squeezing. General anesthesia is suggested for children, terrible eye injuries with cataract, for really worried or uncooperative patients and animals.
Cardiovascular tracking is preferable in local anesthesia and is mandatory in the setting of basic anesthesia. Correct sterile preventative measures are taken to prepare the area for surgery, consisting of use of antiseptics like povidone-iodine. Sterile drapes, dress and gloves are utilized. A plastic sheet with a receptacle helps gather the fluids during phacoemulsification. An eye speculum is placed to keep the eyelids open.
Phacoemulsification Surgical Technique
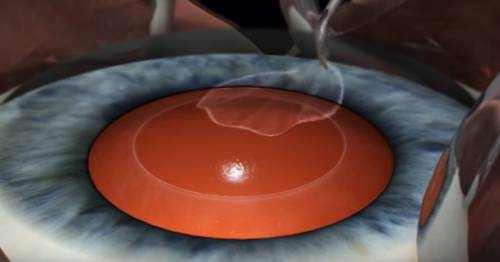
Before the phacoemulsification can be performed, one or more cuts are made in the eye to permit the introduction of surgical instruments. The surgeon then eliminates the anterior face of the pill that contains the lens inside the eye. Phacoemulsification surgery involves the use of a device with microprocessor-controlled fluid characteristics. These can be based on peristaltic or a venturi type of pump.
The phaco probe is an ultrasonic handpiece with a titanium or steel needle. The tip of the needle vibrates at ultrasonic frequency to sculpt and emulsify the cataract while the pump aspirates particles through the suggestion. In some strategies, a second fine steel instrument called a “chopper” is used from a side port to assist with chopping the nucleus into smaller pieces. The cataract is usually burglarized two or 4 pieces and each piece is emulsified and aspirated out with suction. The nucleus emulsification makes it simpler to aspirate the particles. After removing all difficult central lens nucleus with phacoemulsification, the softer outer lens cortex is gotten rid of with suction only.
An irrigation-aspiration probe or a bimanual system is used to aspirate out the staying peripheral cortical matter, while leaving the posterior pill intact. Just like other cataract extraction treatments, an intraocular lens implant (IOL), is put into the remaining lens pill. For implanting a poly( methyl methacrylate) (PMMA) IOL, the incision has to be bigger. For implanting a foldable IOL, the incision does not have to be bigger. The collapsible IOL, made of silicone or acrylic of proper power is folded either using a holder/folder, or an exclusive insertion device supplied along with the IOL.
It is then placed and put in the posterior chamber in the capsular bag (in-the-bag implantation). Often, a ciliary sulcus implantation may be needed since of posterior capsular tears or because of zonular dialysis. Due to the fact that a smaller incision is needed, few or no stitches are required and the patient’s recovery time is typically much shorter when using a foldable IOL.
Phacoemulsification and Intraocular Lens Implantation
Phacoemulsification is a variation of extracapsular cataract extraction, a procedure where the lens and the front part of the capsule are gotten rid of. Formerly the most popular cataract surgery, the older approach of extracapsular extraction includes a longer incision, about 0.4 in (10 mm), or almost half of the eye. Recovery from the bigger cut extracapsular extraction also requires practically a week-long medical facility stay after surgery, and minimal exercise for weeks or even months.
Phacoemulsification Cataract Surgery Risks and Complications
Less than 10 out of 100 people have complications from cataract surgery that could threaten their sight or require more surgery.3 The rate of complications increases in people who have other eye illness in addition to the cataract.
Although the risk is low, surgery for cataracts does include the risk of partial to total vision loss if the surgery is not effective or if there are complications. Some complications can be dealt with and vision loss reversed, but others can not. Complications that may accompany cataract surgery include:
- Infection in the eye (endophthalmitis).
- Swelling and fluid in the center of the nerve layer (cystoid macular edema).
- Swelling of the clear covering of the eye (corneal edema).
- Bleeding in the front of the eye (hyphema).
- Detachment of the nerve layer at the back of the eye (retinal detachment).
Complications that might take place a long time after surgery include:
- Problems with glare.
- Dislocated intraocular lens.
- Clouding of the portion of the lens covering (capsule) that stays after surgery, often called aftercataract (posterior capsular opacification). This is normally not a big problem and can be treated with laser surgery, if required. The kind of IOL may impact how likely it is to have clouding after surgery.
- Retinal detachment.
- Glaucoma.
- Astigmatism or strabismus.
- Sagging of the upper eyelid (ptosis).



