Rheumatoid arthritis is known for joint pain, however it can also impact other parts of the body, including your eyes. Discover which rheumatoid arthritis symptoms and eye concerns are most typical, and how to manage them.
Most people consider rheumatoid arthritis as a joint disease, however like other autoimmune conditions, it can affect various areas of the body too. Among the more typical complications for people with rheumatoid arthritis is eye issues, which can result in corneal damage and eventually impact vision if left neglected.
Rheumatoid Arthritis and Vision Problems
Some common eye conditions, like the ones described listed below, may impact people with rheumatoid arthritis (RA). However there are actions to require to safeguard eye health and avoid irreversible damage.
Dry Eyes
“RA can be connected with extra-articular [suggesting outside the joint] manifestations, and dry eyes are one of the most common problems,” says Ana-Maria Orbai, MD, instructor of medication in the division of rheumatology at the Johns Hopkins University School of Medicine in Baltimore. “An individual with dry eyes may experience itching, a sand-like experience in the eyes, and soreness.” They might likewise notice a lack of moisture or tears in the eyes, in addition to blurred vision.

Although lots of people turn to non-prescription eye drops for relief, the best treatment for dry eyes is prescription drops, which you can obtain from your eye doctor, Dr. Orbai states. A doctor who focuses on treatment of eyes, whereas an optometrist focuses mostly on vision issues, this eye MD can recommend the right type of eye medication for various uses (day versus night, for example).
If you choose to go the over-the-counter route, avoid eye-drop products that have preservatives or vasoconstrictive agents, such as some from Visine and Clear Eyes, which often assure to relieve redness or “take the red out,” Orbai discusses.
If your dry eyes are severe, your doctor may discuss the alternative of punctal plugs, a minor procedure that involves having a little plug inserted into the tear duct to keep the eye from draining pipes. Your doctor may also prescribe Restasis (cyclosporine) drops.
Scleritis
Scleritis is a swelling of the sclera, the white outer layer of the eye. Symptoms can include pain (in some cases severe), swelling, soreness, blurred vision, tearing, and level of sensitivity to light. If you experience any of these issues, you must be examined by your ophthalmologist, Orbai states. And do not delay seeking treatment. “Time is of the essence to prevent eye damage and vision loss,” she states. If it ends up being scleritis, your eye doctor might recommend corticosteroid eye drops and potentially immunomodulator medications, she states.
Iritis and Uveitis
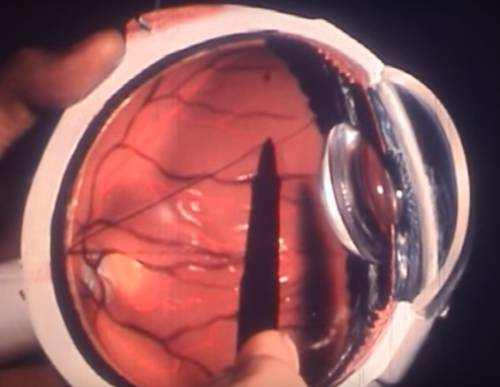
A fast anatomy lesson: The uvea is the middle part of the eye in between the sclera and retina, which is in the back of the eye. The iris is the colored part of the eye that helps manage how much light enters.
Uveitis is an inflammation of the uvea; iritis, a form of uveitis, is an inflammation of the iris. Symptoms include blurred vision; dark, floating spots in your vision; eye pain; soreness; and level of sensitivity to light.
Treatment for either condition depends on the symptoms, Orbai describes. “Some alternatives consist of corticosteroids, Trexall (methotrexate), Humira (adalimumab), and Remicade (infliximab). Your eye doctor will figure out the right course of treatment for you based upon your symptoms.
Medication Complications
A few of the medications used to treat rheumatoid arthritis, such as prednisone (a corticosteroid) and Plaquenil (hydroxychloroquine), can actually activate eye issues. “Plaquenil, on uncommon celebrations, can cause retinopathy,” says Orbai– an inflammatory disease of the retina that can result in disability or loss of vision. And prednisone can cause cataracts or glaucoma, or get worse these conditions if you already have them.
” People who need to take medications that have side effects that impact the eye needs to see an ophthalmologist who can keep track of for adverse results,” states Orbai. “For example, patients using Plaquenil ought to be seen annual to rule out retinopathy.” If they do develop the condition, the doctor might decrease the dosage or stop the medication. “The most essential precaution is to lessen duration of treatment: Take the least quantity for the shortest time,” Orbai states.
The Bottom Line for Your Eyes
Anybody living with RA need to see an eye doctor annual, Orbai suggests. “Only an ophthalmologist can identify and eliminate possible eye issues in people with RA,” she states.
People with RA need to likewise visit an ophthalmologist if they experience any eye symptoms, such as itching, foreign body experience, soreness, pain, or vision loss.
Lastly, it’s important to keep in mind that other conditions like acne and rosacea can lead to eye problems, Orbai explains. It’s good for people with RA to be familiar with this, although it’s still crucial to see your doctor if you’re experiencing any symptoms.