What is blepharospasm? The causes, diagnosis, associated symptoms and treatment methods of blepharospasm will be discussed in this article.
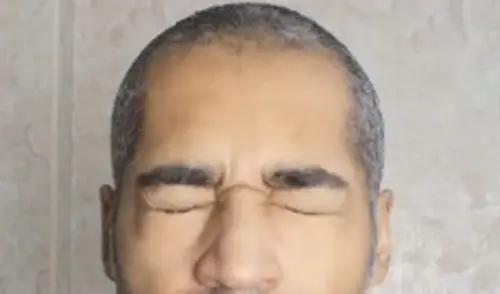
Blepharospasm (blepharo – eyelid, spasm – spasm) is a local neurological disorder in which a person blinks intensely and involuntarily squeezes his eyes. Involuntary contractions of the circular muscles of the eye lead to a persistent spasm and closing of the eyelids. The pectoralis muscle (musculus procerus) and the thinking muscle (musculus corrugator supercilii) are also often involved in the contractions.
According to the International Classification of Motor Disorders, blepharospasm belongs to the dystonia group of hyperkinesias – sudden involuntary movements. It is a facial form of focal dystonia, i.e. dystonia in which only one anatomical region is involved.
Along with cervical dystonia (pathological contraction of the neck and occipital muscles), blepharospasm is the most common form of dystonia. On average, it occurs in no more than 5 people per 100,000 population.
This disorder usually affects people whose profession is associated with increased strain on the eyes: doctors, musicians, typesetters, etc. In most cases patients with this disease live in southern regions with high levels of insolation (sun exposure).
… And women face blepharospasm three times more often than men.
The causes of the disease have not yet been definitively established. Depending on the origin, there are three forms of blepharospasm: congenital, acquired and idiopathic.
Read also about Eye Twitching
Benign Essential Blepharospasm
Benign essential blepharospasm (BEB) is a progressive neurological disorder defined by spontaneous muscle contractions and also spasms of the eyelid muscular tissues. It is a type of dystonia, an activity condition in which muscle contractions cause continual eyelid closure, twitching or repetitive activities.
BEB starts slowly with enhanced regularity of eye blinking often associated with eye inflammation. Other signs may consist of raising problem in keeping the eyes open, and light level of sensitivity.
Typically, the spasms occur throughout the day, disappear in rest, and re-emerge after waking. As the condition progresses, the spasms might magnify, compeling the eyelids to continue to be closed for extended periods of time, and also thereby causing substantial visual disturbance or functional blindness. It is important to keep in mind that the loss of sight is triggered exclusively by the uncontrollable closing of the eyelids as well as not by a disorder of the eyes.
BEB takes place in both males and females, although it is especially usual in middle-aged as well as elderly women.
See also: Eyelid Tics in Adults
Blepharospasm Causes

Congenital blepharospasm is associated with genetic disorders that are transmitted under certain types of inheritance:
- Autosomal dominant – the disease occurs in every generation regardless of gender;
- Autosomal recessive – the disease is transmitted through generations and occurs regardless of sex;
- X-linked recessive – the disease is transmitted through a generation and occurs only in boys (girls become carriers);
- Mitochondrial – the disease is maternally transmitted and occurs in children regardless of sex.
Acquired blepharospasm is caused by other diseases and conditions:
- Damage to the child’s brain in the womb, during childbirth, or during the first week of life;
- Neuroinfections (meningitis, encephalitis);
- drug exposure (levodopa, bromocriptine, dopamine agonists, neuroleptics, metoclopramide, anticonvulsants, antidepressants, calcium channel blockers, SSRIs and antihistamines)
- intoxications (poisoning with cyanide, methanol, manganese, carbon disulfide, cobalt, disulfiram, 3-nitropropionic acid)
- degenerative and vascular diseases of the central nervous system (multisystem atrophy, discirculatory encephalopathy);
- neoplastic processes (brain tumor, paraneoplastic encephalitis);
- craniocerebral trauma;
- functional disorders (psychogenias).
Idiopathic form of blepharospasm occurs due to unspecified reasons.
Good to know: Loss of Peripheral Vision
Symptoms of blepharospasm
More often, blepharospasm occurs in people after the age of 50. Its clinical signs include:
- Difficulty in holding the eyes open. Due to impaired tone of the eye muscles, the patient involuntarily seeks to squeeze, and such spasms occur very frequently.
- Alternating tonic and clonic attacks: spontaneous bilateral rhythmic contractions and relaxations of the eye circle muscles. Spasms intensify with emotional experiences, stressful situations, overexertion, visual tension (reading), watching TV, bright lights, glare from snow or water, cold influences (wind). Symptoms disappear in sleep, are weak upon awakening, alcohol consumption and in a state of hypnosis. Short-term volitional control is preserved.
- Apraxia of eyelid opening – detected in 20-25% of patients. People complain of problems with drooping eyelids. At the same time, patients are able to close and squeeze their eyes shut. This disorder is associated with insufficient activity of the muscles raising the upper eyelids.
- Typical paradoxical actions: reduction or disappearance of blepharospasm when looking down and turning the eyes to extreme external positions, as well as at doctor’s appointments, when eating, when talking and yawning;
- Spontaneous remissions: symptoms of blepharospasm may disappear completely for months or years, even after years of disease.
- A combination or transition to another form of focal dystonia is possible. Classical is the combination of blepharospasm with oromandibular dystonia – involuntary contraction of the muscles of the mouth and lower jaw. Such a combination of dystonias is called Meige’s syndrome. It is manifested by blepharospasm, hyperkinesias in the lower face and/or masticatory muscles. Blepharospasm usually appears first, followed later by oromandibular dystonia.
Diagnosis of blepharospasm
Blepharospasm is diagnosed clinically, i.e. based on the patient’s complaints and objective manifestations of the disease. The diagnostic algorithm consists of the following stages:
- Clinical picture: identification of blepharospasm syndrome and evaluation of its symptoms according to the new Classification of Dystonias 2013 (specifying at what age and for what reason the disease arose, what areas are affected, whether it is combined with other dystonias, etc.)
- Documentation of the clinical picture: video and photo fixation. They help to plan treatment and subsequently evaluate its effectiveness.
- Genetic testing: it is performed if the hereditary nature of blepharospasm is suspected.
Clinical manifestations of the disease are evaluated using standard evaluation scales. The most commonly used scales are the Scott Scale, the Jankovich Scale (JRS), and the Functional Scale of Daily Activity in Blepharospasm (BSDI). They allow to give an objective estimation of the patient’s condition and show the efficiency of treatment in dynamics.
Ball evaluation of visual function in blepharospasm:
- 1 point – blindness;
- 2 points – dependence when outdoors;
- 3 points – independence with poor visual function;
- 4 points – independence with poor visual function;
- 5 points – discomfort;
- 6 points – normal visual function.
Electromyography can confirm functional disorders: blinking patterns and prolonged irregular muscle contractions that lead to forced eye closure. It is not used in real clinical practice, as its results may not correspond to the clinical picture. Usually this method is used in scientific research.
Methods of structural neuroimaging (CT, MRI, functional MRI, etc.) when there is a clear clinical picture of blepharospasm are not recommended for routine diagnosis in adult patients, as their findings may not reveal pathology. MRI of the brain is indicated only as part of the screening of acquired forms of blepharospasm. CT may be needed for differential diagnosis of calcium and iron accumulation in the body.
The differential diagnosis of blepharospasm is made with other similar conditions: myasthenia gravis and myasthenia-like diseases, hemifacial spasm, photophobia, tics, eye opening apraxia, facial neuritis, psychogenic blepharospasm. It is especially important to distinguish blepharospasm from myasthenia gravis, as it is an absolute contraindication for botulinum toxin treatment, which is used for blepharospasm. A distinctive feature of hemifacial spasm is the elevation of the eyebrow due to the spasm of the frontalis muscle – in blepharospasm the eyebrow is pulled into the orbit.
Botulinum toxin type A injection for blepharospasm
The main goal of blepharospasm treatment is to achieve a stable remission with the preservation of patients’ ability to work and social activity.
The “gold standard” in the treatment of blepharospasm is botulinum therapy – local injections of botulinum toxin type A (BTA). This method was originally used by the Californian ophthalmologist A. Scott in the treatment of people with strabismus. A little later, he used local BTA injections to treat patients with blepharospasm and hemifacial spasm. A year earlier ophthalmologist B. Frueh and his colleagues first described the use of BTA in blepharospasm. Since then botulinum toxin has been used not only in ophthalmology but also in the treatment of diseases of the nervous system.
Botulinum toxin therapy became official in 1989 after approval by the FDA (Food and Drug Administration, USA). One of the first indications for the use of BTA was blepharospasm. According to the recommendations of European Federation of Neurology Societies, BTA preparations were recommended as the first line of treatment in this disorder. Their safety and high efficacy has been confirmed by numerous controlled studies and 35 years of clinical practice.
Treatment of blepharospasm
Botulinum toxin is injected into the target muscles: the eyelid muscles and the circular muscles of the eye. If the dosage is observed, the drug eliminates pathological muscle contractions without impairing their function. BTA is recommended to patients immediately after diagnosis. Local injections should be performed regularly. The interval between treatments varies: it all depends on the patient’s well-being. On average, botulinum therapy is performed every 3-4 months.
The effect usually occurs on the 3rd-4th day after the injection and gradually increases. Violent, uncontrolled squeezing ceases, which leads to improvement in vision, as voluntary control of opening and closing of the eyes returns. The effect lasts for 3 to 4 months, sometimes longer. This allows patients to lead a normal life.
Botulinum toxin is produced by the Gram-positive bacterium Clostridium botulinum (botulinum). It affects nerve cells by blocking the release of acetylcholine, a neurotransmitter involved in nerve impulse transmission. This leads to a dose-dependent, reversible decrease in muscle strength.
The dosage is calculated individually according to the instructions for medical use. The unit conversion ratio between Dysport and 100-unit drugs for neurological indications is 3:1 or less, and 2.5:1 for aesthetic indications. The final dosage calculation is left to the physician.
Treatment with botulinum toxin should be performed by experienced professionals with appropriate training. The single point injection dose for 100-unit BTA preparations is 1.25-5 IU. Injections are performed at 3-6 points on each side. The average total dose per side is 15-30 IU, so 30-60 IU of the drug per procedure. Botulinum toxin should not be injected into the middle area of the upper eyelid, as it can lead to ptosis (drooping eyelid).
Possible side effects of BTA:
- very often – ptosis;
- frequent – weakness of facial muscles, diplopia (double vision), dry eyes, eyelid swelling, lacrimation;
- infrequent – paresis of facial muscles;
- rarely – ophthalmoplegia (lesion of the oculomotor nerves), eyelid screwing.
To reduce the risk of adverse events, it is important to observe the dose of BTA, start treatment with the lowest effective dosage. Drugs that affect nerve impulse transmission, such as aminoglycoside antibiotics (amikacin, gentamicin, etc.), should be used with caution.
Before performing botulinum therapy, it is mandatory for the doctor to execute a voluntary informed consent for the injections. After BTA injections, it is recommended to actively contract the injected muscles for 20 min and to be under medical supervision for one hour to monitor the occurrence of immediate allergic reactions. To reduce the risk of intradermal bruising of the face, it is recommended to cool the injection sites for 10-20 minutes.
Another effective way to eliminate the symptoms of blepharospasm are pink sunglasses (with FL-41 filter). They are used to avoid provocation of squinting.
Drug therapy for blepharospasm is a thing of the past, but if BTA is not possible, the following drugs can be prescribed: dopaminergic, cholinergic, serotoninergic, catecholamines, GABA, anticonvulsants, benzodiazepines, neuroleptics. Their effectiveness does not exceed 20%, is often temporary, and requires a step-by-step increase in dose and prolonged administration. Clonazepam and baclofen are the most frequently prescribed medications. However, it should be remembered that many drugs have side effects, including addiction.
Myorelaxants (tolperizone, tizanidine), benzamides (sulpiride, thiapride) and antidepressants (amitriptyline, fluoxetine, paroxetine, sertraline, fluvoxamine, trazodone) and anxiolytics (anti-anxiety medications) have the least effect. They are prescribed as an adjunct to other medications for correction of concomitant pathologies (pain syndrome, emotional and/or somatoform disorders).
Blepharoplasty, an operation to remove excess skin and soft tissues of the upper eyelid, can be used as an additional method of treatment. It improves the tolerance and results of BTA injections.
Deep brain stimulation (implantation of a special device that sends electrical impulses to the right part of the brain) has shown little efficacy in blepharospasm. In addition, there is the possibility of postoperative side effects: speech disorders, paresthesias, development of hypokinesia, coordination disorders, infection, malfunction of the implanted generator, electrode damage. This procedure can be considered if there is no effect after 3-6 BTA procedures in a sufficient dose, i.e. in case of resistance to BTA, which is extremely rare. Other surgical methods of blepharospasm correction are insufficiently effective and traumatic.
It is necessary to pay special attention to socialization and adaptation of the patient: to include him in psychological support groups, psychotherapy and cognitive-behavioral therapy.
Prognosis and Prevention
With regular treatment of blepharospasm, spontaneous remission can be achieved for many years, but one should not forget about the high probability of relapse.
For prevention, you should optimize the conditions at your workplace, especially for people working with an increased load on the visual apparatus. It is important to observe a rational mode of work and rest, regularly perform moderate physical activity, avoid stress overloads, trauma and painful manipulations on the head and neck, including chiropractic care.
Used sources:
- Molloy A., Williams L., Kimmich O., et al. Sun exposure is an environmental factor for the development of blepharospasm // J Neurol Neurosurg Psychiatry (link).
- Simpson D., Hallett M., Ashman E., Comella C., et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology // Neurology (link).
- Hallett M. Blepharospasm: recent advances // Neurology (link).
- Albanese A., Lalli S. Is this dystonia? // Mov Disord (link).
- Meunier S., Lehericy S., Garnero L., Vidailhet M. Dystonia: lessons from brain mapping // Neuroscientist (link).
- Frueh B., Felt D., Wojno T., Musch D. Treatment of blepharospasm with botulinum toxin. A preliminary report // Arch Ophthalmol (link).
- Ho R., Fang P., Chao T., Chien C., Kuo M. Increase lipid tear thickness after botulinum neurotoxin A injection in patients with blepharospasm and hemifacial spasm // Sci Rep (link).





