A corneal abrasion (scratched cornea or scratched eye) is among the most typical eye injuries. A scratched cornea often causes substantial pain, red eyes and hypersensitivity to light. Corneal abrasions arise from a disruption or loss of cells in the top layer of the cornea, called the corneal epithelium.
The cornea is the clear front surface area of the eye, and part of its job is to focus light, enabling you to see. A healthy cornea is essential for excellent vision. In addition to interfering with vision, a scratched cornea makes your eye more vulnerable to infection. So it is very important that you see your optometrist or visit an emergency clinic or immediate care center as soon as possible if you suspect you have a corneal abrasion.
If you have a corneal abrasion, your ophthalmologist might patch your eye so that you are more comfy. You may also be offered medication to decrease the pain. Using sunglasses might likewise lessen the symptoms of corneal abrasion while you are recovery.
What Causes Corneal Abrasions?
There are many methods to obtain a corneal abrasion. No matter how big or little, anything that makes contact with the surface of your eye can cause injury.
Tree branches, paper, makeup brushes, an animal, a finger, workplace debris, sports devices and more all pose a risk to the front surface area of your eyes.
Many corneal abrasions aren’t triggered by a visible traumatic occasion, such as getting poked in the eye. Sand, dust and other little particles can cause a corneal abrasion also, specifically if you rub your eyes.
Dry eyes can increase your risk of a corneal abrasion, particularly when awakening from sleep. If your eyes dry out while you are sleeping, your eyelids may adhere to your cornea. When you wake up and open your eyes, your lids can tear and remove a part of the external layer of the cornea (epithelium), triggering a painful abrasion.
Contact lenses typically won’t safeguard your eyes from corneal abrasions. In reality, if your contacts are harmed or you use them too long, they may even increase your risk of a scratched cornea.
Symptoms Of A Scratched Cornea
The cornea is one of the most delicate parts of your body, so even a really little corneal abrasion can be incredibly painful and feel much bigger in size– as if you have a huge, rough things in your eye.
In addition to pain and a gritty or foreign body feeling, other symptoms and signs of corneal abrasions consist of soreness, tearing, light sensitivity, headache, blurred or decreased vision, eye twitching, a dull pains and, periodically, nausea.
If you believe you may have suffered a corneal abrasion and are experiencing any of these symptoms, look for medical attention right away.
Why Do Corneal Abrasions Hurt So Much?
The cornea has lots of nerve cells. Cells called pain receptors to transmit pain to inform us about possible damage to the eye’s surface area. There are numerous times more pain receptors in our cornea than there remain in our skin.
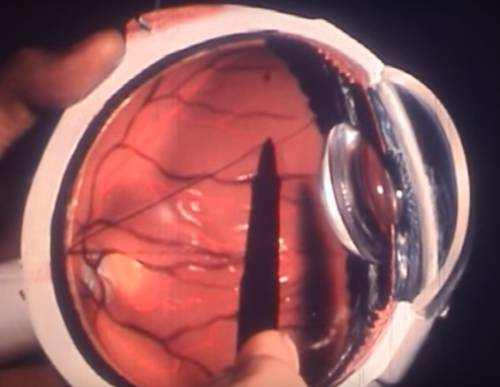
Corneal Abrasion Diagnosis
Your eye doctor will put color called fluorescein on your eye’s surface. Then they will take a look at your cornea with an instrument called a slit light. The dye will highlight a cut or scratch on the cornea.
What To Anticipate
Individuals have a tendency to rub their eyes when they feel like something is “in” them, however this can make matters much worse. If you get something in your eye, you can attempt to flush it out with water, however don’t rub your eye. Do not spot it either, because this can speed bacterial growth and increase the risk of an eye infection.
If possible, rinse your eye with a sterile saline eye wash or a multipurpose contact lens option instead of faucet water or mineral water. Bacteria such as Acanthamoeba have actually been discovered in faucet water as well as bottled water, and these pathogens can cause a major, vision-threatening infection if presented to an eye with a scratched cornea.
After flushing the eye, if soreness, pain or foreign body experience continues, look for immediate attention since corneal abrasions can cause serious harm in just 24 hours.
To detect a corneal abrasion, your eye doctor or eye doctor may apply an eye drop to numb your eye so you can keep it open for the examination. Another kind of eye drop might be used to assist your doctor see the level of the abrasion when viewing your eye with a blue light and an analyzing microscopic lense called a slit lamp.
Depending upon what may have triggered the scratch and what your doctor sees during the test, your eye may be gently swabbed for a culture to ensure correct treatment in case of infection.
Treatments For A Corneal Abrasion
Treatment for a corneal abrasion depends upon the seriousness of the injury and the cause. Minor abrasions in some cases can be treated with non-preserved lubricating drops to keep your eye moist and comfortable while your eye’s natural healing procedure takes place.
As a precaution, even shallow abrasions sometimes are likewise treated with antibiotic eye drops to prevent infection during recovery.
Superficial corneal abrasions tend to recover rapidly, normally within two or three days.
However other corneal abrasions might require an antibiotic ointment that stays on the eye longer, a steroid to decrease inflammation and scarring, and something to ease pain and light level of sensitivity. Large, deep corneal abrasions take longer to recover and can cause a permanent scar that might affect vision.
In many cases, scratched corneas are treated with what’s referred to as a bandage contact lens. When used with prescription eye drops, these unique lenses offer pain relief and sometimes can speed recovery.
Normally, routine contact lenses should not be used over a corneal abrasion due to the fact that of increased risk of an infection developing under the lens. Your eye doctor will inform you when it’s safe to resume using your contacts following a scratched cornea.
Depending on the treatment and seriousness of the injury, your optometrist or eye doctor might set up a follow-up test as soon as 24 Hr after preliminary treatment.
When dealt with right away, most corneal abrasions result in a complete recovery with no permanent vision loss. But some much deeper abrasions that take place in the center of the cornea (straight in front of the student) can leave a scar and lead to a loss of visual skill.
If left without treatment, some deep corneal abrasions can cause a corneal ulcer that can cause severe vision loss. Abrasions triggered by raw material, in specific, can increase the risk of corneal ulcer.
Attending your follow-up appointments is essential, because corneal abrasions do not always recover correctly and can lead to frequent corneal disintegrations and other complications that can impact your vision and convenience.
What is the Prognosis of a Corneal Abrasion?
The prognosis is typically excellent, with full recovery of vision if treatment is prompt; nevertheless, without treatment, corneal abrasions can cause blinding corneal ulcers.
Some deep abrasions (e.g., those involving the corneal stromal layer) in the central visual axis (i.e., the primary area of the cornea straight over the pupil) heal but leave a scar. In these instances, an irreversible loss of visual skill might arise from corneal cloudiness or irregular corneal astigmatism.
Recovery of small abrasions is expected within 24-48 hours. Substantial or deep abrasions may need a week to heal.
How To Prevent A Scratched Eye
Although lots of causes of corneal abrasions are hard to avoid, others can be avoided by taking some basic, common-sense safety measures.
For instance, always wear shatterproof glass or protective goggles in work environments with airborne debris, especially in welding environments. Also, protective eyewear ought to be used when doing backyard work, utilizing power tools, and playing sports.
If you wear contact lenses, always follow your eye doctor’s instructions concerning how long to wear them, when to discard them, and the proper contact lens care options to use to assist keep your corneas healthy and strong.
If you experience a corneal abrasion that seems connected to dry eyes, see your optometrist for an in-depth examination of the front surface area of your eyes and, if needed, follow the dry eye treatment protocol your doctor recommends.
Corneal Abrasion Questions & Answers
What are the possible complications of corneal abrasions?
Most people recuperate entirely from minor corneal abrasions without long-term eye damage. However, much deeper scratches can result in corneal infections, corneal erosion, or scarring of the cornea. If not treated correctly, these issues can result in long-lasting vision problems. Any unusual symptoms, including a reoccurrence of pain following recovery, must be reported to your optometrist.
What are the causes of foreign body-related corneal abrasions?
Foreign body-associated abrasions are flaws in the corneal epithelium that arise from removal or spontaneous dislodgement of a corneal foreign body. Foreign body abrasions usually are brought on by pieces of metal, wood, glass, plastic, fiberglass, or veggie product that have ended up being ingrained in the cornea or adherent to the inner surface area of the upper lid.
What are contact lens-related corneal abrasions?
Contact lens-related abrasions are problems in the corneal epithelium that are left behind after the removal of an overworn, improperly fitting, or improperly cleaned contact lens. In these cases, the mechanical insult is not from external injury; however, instead of from a foreign body that may be related to specific pathogens.
Which patients are at threat for spontaneous corneal abrasions?
Spontaneous problems in the corneal epithelium might accompany no instant antecedent injury or foreign body. Eyes that have suffered a previous terrible abrasion or eyes that have an underlying problem of the corneal epithelium are vulnerable to this problem.
What is the conjunctival reaction to corneal abrasion?
The conjunctival reaction to corneal wounding has been understood considering that 1944 when Mann first observed that peripheral corneal abrasions recover by the moving of limbal cells to cover the epithelial flaw. This reaction is divided into two stages:
- the response of the limbal epithelium, which is the source of the new corneal epithelial stem cells, and
- the reaction of the conjunctival epithelium itself.
Under normal circumstances, the limbal epithelium functions as a barrier and exerts a severe growth pressure that avoids the migration of conjunctival epithelial cells onto the cornea. Like the remainder of the surface area of the body, the conjunctiva and the cornea remain in a consistent state of turnover. Corneal epithelial cells are continually shed into the tear pool, and they are simultaneously replenished by cells moving centrally from the limbus and anteriorly from the basal layer of the epithelium.
Motion from the basal to superficial layers is relatively rapid, requiring 7-10 days. Nevertheless, movement from the limbus to the center of the cornea is slow and might require months.
This normal physiologic process is overemphasized when it comes to a corneal abrasion. During corneal healing of a lesion, corneal epithelial cells end up being flattened, they spread, and they cross the defect up until they cover it completely. Cellular expansion, which is independent of cell migration, starts around 24 hours after injury.
Stem cells from the limbus also respond by increasing to generate daughter cells called transient enhancing cells. These cells migrate to heal the corneal flaw and grow to replenish the injured area. The observation of limbal pigment migrating onto the clear cornea supplies extra proof of this procedure.
How does the regrowth of corneal epithelium happen in the pathophysiology of a corneal abrasion?
Rearrangement of intracellular actin filaments plays a role in motion. Cell migration can be inhibited by obstructing polymerization of actin, indicating that actin filaments actively take part in the mechanism of cell motion. Some authors believe that conjunctival and limbal epithelial cells might add to the regeneration of corneal epithelium. Marked proliferative reactions in the conjunctiva after a central corneal epithelium abrasion have been explained.
How does the size of the wound impact the pathophysiology of corneal abrasions?
The magnitude and extent of both the conjunctival and corneal regenerative responses to a corneal abrasion correlate with the size of the wound. Big epithelial problems were reported to induce a noticeable action on the rate of epithelial cell migration and mitosis at the limbus.
Insults caused by chemical injuries, Stevens-Johnson syndrome and contact lens-induced keratopathy may lead to limbal damage. These insults trigger delayed recovery of the cornea, frequent epithelial erosions, corneal vascularization, and conjunctival epithelial ingrowth.
What is sports-related corneal abrasion?
Corneal abrasions can occur in nearly all sports. They most often happen in youths.
In places where soccer is played often, impact with the soccer ball triggers around one-third of all sports-related eye injuries. Contrary to previous ophthalmologic mentor that balls bigger than 4 inches in size hardly ever cause eye injury, 8.6-inch soccer balls trigger most soccer-related eye injuries, both severe (e.g., hyphema, vitreous hemorrhage, retinal tear, chorioretinal rupture, angle recession) and minor (e.g., corneal abrasions, wounds).
Approximately 1 in 10 college basketball players has an eye injury each year. A lot of basketball-related eye injuries are corneal abrasions caused by an opponent’s finger or elbow striking the player’s eye.
The occurrence of extreme eye injuries in fumbling is low. In a study at Michigan State University, 18.4% of wrestlers had reasonably mild eye injuries (e.g., lacerated eyebrows, corneal abrasions) and that left no long-term damage. The typical college team with 25 gamers and 2600 direct athlete exposures ought to expect 1-2 eye injuries each season, with a significant injury every 9-10 seasons.
Although significant eye injuries are not a significant risk in equestrian events other than polo, cross-country riders often have corneal abrasions from striking tree branches overhanging the trail. Using eyeglasses with polycarbonate lenses provides appropriate security against this danger.
Although cross-country snowboarding causes less musculoskeletal injuries than alpine snowboarding, cross-country skiers are most likely than alpine skiers to have eye injuries, particularly corneal abrasions from contact with tree twigs. Also, both cross-country and downhill skiers can have solar keratopathy (snow loss of sight) and injuries due to mishaps with ski poles.
What is the incidence of corneal abrasion due to general anesthesia?
General anesthesia is more likely to trigger adverse systemic results than local or ocular problems. Ocular issues that do happen are usually not severe and include corneal abrasion, chemical keratitis, hemorrhagic retinopathy, and retinal anemia (unusual).
The incidence of corneal abrasion due to the necessary anesthesia is as high as 44%. Basic safety measures, such as instilling a boring ointment or taping both sets of eyelids closed in the case of non-ocular surgery and the covers of the nonoperative eye in the case of ocular surgery, might prevent surface area injury produced by the surgical drape, anesthetic mask, or direct exposure and drying of the cornea. Reduced tear production under general anesthesia, proptosis, and a bad Bell phenomenon might worsen direct corneal exposure, requiring eyelid suturing in some prone patients.
What is the frequency of corneal abrasions in the US?
Corneal abrasions are the most typical eye injuries and are specifically widespread amongst individuals who wear contact lenses. Although corneal abrasions represent about 10% of eye-related emergency visits, the estimated occurrence varies by population and depends upon how they are specified, and the activities involved in the mechanism of injury.
A tasting of medical diagnoses in the offices of family practice clinicians, internists, and pediatricians in the United States in 1985 discovered that eye complaint made up 2% of all patient checkouts; terrible conditions and foreign bodies were the reason for 8% of these checkouts.
Workplace eye injuries cause significant yet preventable (with protective glasses) morbidity and lost efficiency. In the United States, 65,000 work-related eye injuries and diseases that trigger missed out on time from work take place each year.
A research study of eye injuries in a significant US vehicle corporation discovered a yearly incidence of 15 eye injuries per 1000 employees. In between July 1989 and June 1992, an overall of 1983 work-related eye injuries took place at 33 plants, with 86.7% of cases being superficial foreign bodies and corneal abrasions. The eye injuries comprised 6% of overall injuries. One-third of eye injuries failed workers to resume normal responsibilities for a minimum of 1 day.
In another report, many patients with corneal foreign bodies did not take more than one day off work, and as much as 30% sought treatment beyond working hours to prevent lost time from work.
How does the incidence of corneal abrasions vary by race, sex, or age?
Rates of corneal abrasion are equal in all races. More males than females are treated for corneal abrasions.
The occurrence of corneal abrasion is higher amongst individuals of working age. Nevertheless, people of any ages can have a corneal abrasion. Automotive workers between the ages of 20 and 29 years had the highest occurrence of eye injuries.
What is the basis for treatment selection for corneal abrasion?
Identifying the best treatment for a corneal abrasion depends upon many elements, such as the seriousness of the injury and the degree of pain the client is experiencing. But professionals likewise must take into consideration the location of the abrasion, symptoms the patient may be displayed, and how the incident happened. Was it merely a scratch or a shearing injury that tore the epithelium away from the underlying basement membrane? Was it triggered by a plant-type product, a circumstance in which a later on fungal infection might be possible?
The level of pain also figures in the treatment strategy. Furthermore, pain affects everybody in a different way, so pain management must be customized to each person. 2 patients with substantially similar injuries or injuries might explain the pain level very in a different way. It is essential to understand that pain is private. When attempting to manage pain associated with corneal abrasion, the pain management approach should be based on the client’s pain rather than the patient’s injury.
Any symptoms that a client may display also helps choose the course of treatment. If the patient is experiencing substantial sensitivity to light or excessive lacrimation, she or he ought to be dealt with differently from somebody who has a little abrasion with small symptoms. It also depends on the place of the injury. If it is central, the treatment strategy ought to be more aggressive than if the injury is peripheral.
As the demand for refractive surgery grows, practitioners are most likely to see different kinds of corneal abrasions originating from a surgery. Refractive surgery has rekindled the interest in treating corneal abrasions because lots of post-refractive surgery patients develop some mild degree of what would be considered an abrasion. Photorefractive keratectomy by external triggers a relatively significant epithelial defect, which exceeds just an abrasion. In laser in situ keratomileuses (LASIK), although there is not a huge area of open abrasion, there are peripheral areas of the cornea where the flap edge might show a circumferential pattern of superficial punctate keratitis surrounding to the microkeratome cut. Numerous eye doctors have reacquainted themselves with this, in regards to refractive surgery offering unusual appearing iatrogenically created abrasions that do not always totally heal.
How is recurrent erosion avoided during the treatment of corneal abrasion?
While keeping an eye on the cornea for signs that the tissue is healing, a boring lubricating ointment for 6-8 weeks to lower the potential for frequent erosion or a hypertonic lotion, depending on the appearance of the cornea, must be considered.
Hyperosmotic agent ointment (sodium chloride 5%) every night, in addition to a daily hypertonic drop, for 60 days must be thought about.
If frequent erosion can be prevented, the patient has been well served. Reoccurring erosion can end up being a lifelong issue. Numerous patients with persistent erosion ultimately need laser procedures or corneal stromal micropuncture.
Unsettled corneal erosions present a challenge in terms of treatment.
What is the role of prophylactic antibiotics for non-infected corneal abrasions?
To the authors’ understanding, no randomized, double-blind placebo-controlled trials have been conducted to assess the benefit of prophylactic antibiotics for non-infected corneal abrasions. Since the incidence of microbial keratitis in this setting is low, such a research study is unlikely. The estimated yearly incidence of ulcerative keratitis is 0.13-0.21% for people who wear extended-wear soft contact lenses and 0.02-0.04% for those using daily-wear soft contact lenses.
You can leave your comment about Corneal Abrasion below.