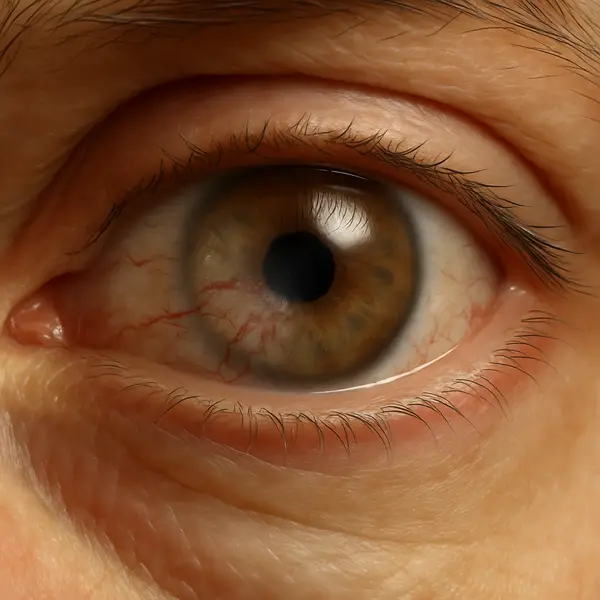
Corneal neovascularization (CNV) is a condition where new, abnormal blood vessels invade the cornea — the normally clear, avascular (without blood vessels) front layer of your eye. These vessels can cloud vision, cause discomfort, and, in some cases, lead to serious complications. Think of it as an uninvited guest showing up at your front porch with muddy boots.
Don’t ignore the little things—your eyes are smarter than they look.
Your view might look foggy or slightly out of focus, especially when blinking or in bright light.
Bright lights suddenly become harsh or uncomfortable—yes, even your phone screen.
Feels like there’s sand in your eye, even when nothing’s there. Annoying? Definitely.
Not fire-engine red, but just enough to make your eye look tired or irritated in the mirror.
Your eye starts tearing up randomly, not from emotion—but it might be sending you a message.
If a minor eye injury takes longer than usual to heal, abnormal vessel growth might be interfering with recovery.
This invasion usually results from a lack of oxygen (hypoxia) or inflammation. The cornea, which gets nutrients from the tear film and aqueous humor, responds to oxygen deprivation by triggering growth signals, particularly vascular endothelial growth factor (VEGF), prompting new vessel formation. It’s the eye’s desperate SOS signal — unfortunately, it does more harm than good.
Common Causes: Why Blood Vessels Start Creeping In
The most frequent culprits of corneal neovascularization include:
- Contact lens overwear: Wearing lenses longer than recommended — especially low-oxygen types — reduces the oxygen available to the cornea. Think of it like putting plastic wrap over a window: light still gets in, but air can’t circulate. This lack of oxygen causes the eye to panic and grow new vessels. You might notice redness, discomfort, and a feeling like something is stuck in your eye.
- Infections: Conditions like herpes simplex keratitis or bacterial ulcers damage the corneal surface, triggering inflammation. When this tissue is under attack, the body tries to deliver immune cells by forming new vessels — but that does more harm than good in the cornea. Symptoms can include pain, light sensitivity, blurry vision, and discharge.
- Trauma: Injuries like chemical burns or physical abrasions disturb the corneal structure. When healing, the eye may overcompensate by growing new blood vessels to the area. If you’ve experienced sudden eye pain, watering, or vision changes after an accident, trauma may be the hidden trigger.
- Autoimmune conditions: Diseases like Stevens-Johnson syndrome or ocular cicatricial pemphigoid cause long-term inflammation of the eye’s surface. The immune system essentially mistakes healthy eye tissue for a threat. Chronic redness, irritation, and scarring can be early signs that autoimmunity is driving CNV.
- Surgical interventions: Procedures such as LASIK or corneal grafts, while often beneficial, can sometimes lead to unintended inflammation. The healing process may spark vessel growth as the eye attempts to rebuild itself. Blurred vision or redness weeks after surgery may signal this complication.
One striking case from Phoenix, AZ involved a 32-year-old male contact lens wearer who slept in his lenses for weeks at a time. He developed blurred vision and a gritty sensation. A slit-lamp exam revealed deep stromal neovascularization. His condition improved after lens discontinuation and anti-VEGF therapy.
How Is CNV Diagnosed?
Eye care professionals rely on several diagnostic methods to assess the extent and depth of CNV:
1. Slit-Lamp Biomicroscopy
- How it works: Uses a high-intensity light beam and microscope to view corneal layers. The patient rests their chin and forehead on a support while the ophthalmologist examines the eye under magnification. The procedure is completely painless and takes just a few minutes. You might feel a bright light, but there’s no contact with the eye.
- Accuracy: 6/10 for depth, 8/10 for surface vessel detection.
- Cost: Typically $80–$150 in the U.S.
2. Fluorescein Angiography (FA)
- How it works: A dye is injected into the bloodstream, highlighting vessels under special light. A technician injects fluorescein dye into your arm, and as it circulates through your eyes, images are taken rapidly. The test is mostly painless, though some people experience a mild warm sensation or temporary nausea. It takes about 10–20 minutes, and the dye may cause your skin or urine to appear yellow temporarily.
- Accuracy: 9/10 for both surface and deep vessel mapping.
- Cost: $300–$500
3. Anterior Segment Optical Coherence Tomography (AS-OCT)
- How it works: Non-invasive imaging that provides cross-sectional views of the cornea. You sit in front of the device, and it scans your eye using harmless light waves — no touch, no discomfort. The process takes less than five minutes and requires no preparation or recovery. It’s similar to taking a photograph of your cornea in super-high resolution.
- Accuracy: 8.5/10 for vessel depth and corneal thickness.
- Cost: Around $250–$400
Recent innovations like ultra-high-resolution OCT are improving early detection, especially in subclinical CNV cases ⧉
Current and Emerging Treatment Options
Managing CNV focuses on halting vessel growth, restoring clarity, and treating underlying causes. Here’s what’s in the toolbox:
1. Anti-VEGF Injections
- Example: Bevacizumab (Avastin)
- How it works: VEGF (vascular endothelial growth factor) is a key molecule that tells the body to grow new blood vessels. Anti-VEGF drugs bind to this molecule and block its activity, essentially telling the eye to stop growing vessels where they don’t belong.
- Application: Usually given as a subconjunctival injection — a small needle delivers the medication just under the thin membrane covering the white of the eye. Most patients require a series of 2 to 3 injections spaced a few weeks apart, depending on severity.
- Cost: Each injection session can cost between $300–$700 without insurance, and follow-ups may add another $150–$200.
- Efficacy: Shown to regress neovascularization in 65% of cases within 4 weeks ⧉
2. Topical Steroids
- Common drugs: Prednisolone acetate, loteprednol ⧉
- How it works: These drops reduce inflammation by calming the immune response that contributes to abnormal vessel growth. By lowering inflammation, the cornea is less likely to trigger vessel development.
- Application: Typically prescribed as drops used 2–4 times daily for 1 to 3 weeks, with adjustments based on response.
- Cost: A standard 5ml bottle ranges from $50–$120. Longer treatment may require multiple refills and follow-ups.
- Efficacy: Effective in early-stage or mild CNV cases, with partial regression seen in 40–60% of patients.
3. Laser Photocoagulation
- Device: Argon laser.
- How it works: A focused beam of light is used to cauterize (burn) the abnormal blood vessels in the cornea. This prevents them from carrying blood, which halts further growth and can shrink the vessels over time.
- Application: Performed in-office under topical anesthesia. The session typically lasts 15–30 minutes, and patients may require 1 to 2 treatments based on vessel depth.
- Cost: The procedure can cost between $500–$1,200, including the initial consultation and post-op care.
- Efficacy: 70–80% success rate in reducing or halting progression, particularly in superficial vessel cases.
4. Surgical Treatments
- Methods: Fine-needle diathermy or corneal transplantation.
- How it works: Diathermy uses a heated needle to seal off blood vessels, while corneal transplants replace damaged tissue with healthy donor cornea. Both aim to restore corneal clarity and halt vessel progression.
- Application: These are outpatient procedures requiring local or general anesthesia. Diathermy is quicker (20–30 minutes), while transplantation is more intensive and involves weeks of recovery.
- Cost: Diathermy ranges from $800–$1,500; corneal transplantation may cost $7,000–$12,000 in total, including surgery, donor tissue, and follow-up.
- Efficacy: Diathermy offers regression in 60–70% of localized CNV cases. Corneal transplants restore vision in over 80% of advanced cases, though recurrence is possible.
Reyus Mammadli, medical consultant, recommends combining anti-VEGF therapy with steroids for stubborn cases, noting that “dual therapy offers a synergistic effect, especially in post-infectious CNV.”
Step-by-step journey through diagnosis and treatment — clear, practical, and not as long as you think.
Day 1 – Slit-lamp exam and OCT imaging confirm CNV; eye doctor evaluates severity and layer depth.
Days 2–3 – Based on findings, topical steroids or anti-VEGF injections are prescribed. In some cases, both.
Week 1 – First subconjunctival injection (e.g., Avastin) or initiation of steroid drops (4x/day for 2–3 weeks).
Week 3–4 – Eye exam to assess regression of vessels; further imaging may be performed.
Week 4–6 – Second injection (if needed) or tapering steroids; switch treatment if response is low.
Monthly – Regular check-ups every 4–6 weeks for up to 6 months. Most patients stabilize within 8–12 weeks.
Prevention: Don’t Wait Until It’s Too Late
If you’re wearing contact lenses, your eye health depends on good habits:
- Use high oxygen-permeable lenses (e.g., silicone hydrogel): These lenses allow much more oxygen to reach the cornea compared to older soft lenses. Daily wear lenses made of silicone hydrogel reduce the risk of CNV by up to 50% in long-term users.
- Follow the replacement schedule strictly: Don’t try to squeeze a few more days out of your lenses — worn lenses lose their structure and oxygen permeability. Most cases of lens-related CNV involve patients who extended use far beyond manufacturer guidelines.
- Never sleep in your lenses unless specifically prescribed: Overnight wear is the fastest way to cut off oxygen supply to your cornea. Even with approved lenses, overnight wear increases the risk of complications like CNV by ⧉.
- Schedule regular eye exams (every 6–12 months): Early vessel growth can only be detected through slit-lamp exams or OCT imaging. A yearly check-up with your optometrist can catch problems before they escalate into permanent damage.
For those with chronic eye diseases, consistent monitoring and anti-inflammatory treatments can reduce CNV risk by up to 40% ⧉ .
Who’s at Risk?
CNV can affect anyone, but some groups are more vulnerable:
- Contact lens users (especially extended-wear types): Wearing lenses for too long reduces oxygen supply to the cornea — a key trigger for neovascularization. Studies show that up to 30% of chronic lens users exhibit early signs of vessel growth.
- Post-surgical patients (LASIK, corneal transplants): Any surgery on the cornea can initiate an inflammatory response, increasing the likelihood of abnormal vessel formation. While less common than contact-lens-related cases, post-surgical CNV occurs in 10–15% of complicated procedures.
- People with chronic blepharitis or dry eye: Persistent inflammation on the ocular surface disrupts normal corneal defenses and oxygen exchange. These patients may not notice symptoms until vessels are already present.
- Individuals in polluted or dry environments (e.g., Las Vegas, NV): Harsh environmental conditions lead to frequent dryness, irritation, and microtrauma to the cornea. Though indirect, this risk factor is notable in regions with arid climate and poor air quality.
Source: eyexan.com
A 45-year-old woman from Chicago with long-term dry eye syndrome developed peripheral neovascularization after skipping follow-up visits. Early detection and lubricating drops stabilized her vision. Moral of the story? Your eyes aren’t low maintenance.
Helpful Table: CNV Diagnostic Methods At a Glance
| Diagnostic Tool | Accuracy | Invasiveness | Average Cost (USD) | Best For |
|---|---|---|---|---|
| Slit-Lamp Biomicroscopy | Medium-High | Non-invasive | $80–150 | Surface vessels |
| Fluorescein Angiography | High | Invasive | $300–500 | Detailed vessel mapping |
| AS-OCT | High | Non-invasive | $250–400 | Deep vessels and corneal layers |
Editorial Advice
Reyus Mammadli, medical consultant, emphasizes the importance of early intervention: “Once vessels enter the cornea, they rarely disappear on their own. Catching CNV early is key to protecting long-term vision.”
Avoid over-the-counter drops unless advised, and steer clear of home remedies. Trust your ophthalmologist, not the internet. Staying proactive with eye care is the best defense.
And remember: if your eyes start seeing red (literally or figuratively), it’s time to give them some TLC — Tender Loving Cornea care.



