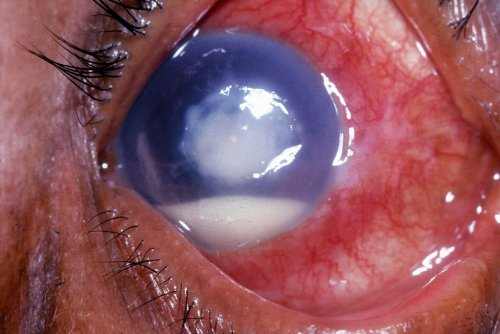
A corneal ulcer generally takes place as a painful, red eye, with mild to severe eye discharge and decreased vision. The condition arises from a localized infection of the cornea, just like an abscess.
Causes Of Corneal Ulcer
A lot of cases of corneal ulcer are because of a bacterial infection that attacks the cornea — frequently following eye injury, trauma or other damage.
Contact lens users especially are susceptible to eye irritation that can lead to a corneal ulcer. A contact lens might rub against the eye’s surface, producing minor damage to the epithelium that might enable bacteria to penetrate the eye.
If you are a contact lens wearer, you can increase your opportunities of preventing a corneal ulcer by practicing good health such as washing your hands prior to handling lenses and following other safety pointers.
Besides bacterial infection, other causes of corneal ulcers are fungis and parasites, such as:
- Fusarium. These fungi have actually been connected with fungal keratitis outbreaks amongst contact lens wearers who used a specific kind of contact lens option. Now withdrawn from the marketplace, this contact lens solution formerly cannot avoid this type of infection.
- Acanthamoeba. These common parasites can enter the eye and cause Acanthamoeba keratitis, an extremely severe eye infection that can result in long-term scarring of the cornea and vision loss. Acanthamoeba microorganisms are frequently found in tap water, pool, hot tubs and other water sources.
Contact lens wearers who cannot remove their lenses before swimming significantly increase their risk for a corneal ulcer from Acanthamoeba keratitis.
Another reason for corneal ulcer is herpes simplex virus infection (ocular herpes), which can damage outside and often even deeper layers of the eye’s surface area.
See also: Bacterial, Fungal and Viral Eye Infections
Other underlying causes of corneal ulcers are severely dry eyes, eye allergies and extensive general infection. Immune system conditions and inflammatory illness such as several sclerosis and psoriasis likewise can lead to corneal ulcers.
Diagnisis and Treatment of Corneal Ulcers
Your essential step if you suspect you have a corneal ulcer is an immediate check out to your eye doctor. Otherwise, neglected corneal ulcers can result in severe vision loss as well as loss of the eye.
If your doctor presumes that bacteria are the cause of your corneal ulcer, normally treatment consists of regular application of topical antibiotics, with or without preliminary cultures.
The area and size of the ulcer will guide your eye doctor in determining the need for cultures. A lot of optometrist see patients with corneal ulcers each to 3 days, depending upon the intensity of the condition.
If the ulceration is in the main cornea, the condition typically takes longer to disappear, and vision may be decreased permanently due to scarring. Sadly, long-term damage and vision loss may occur even if the condition is identified and treated early.
If you have experienced injury to the eye, your doctor might suspect ulceration from fungal keratitis, especially when your eye has actually come across raw material such as from a tree branch.
In most cases of this type of corneal ulcer, the eye already is compromised by pre-existing conditions, such as an immune disorder.
Your doctor would diagnose fungal keratitis just with microscopic assessment of specially stained specimens or cultures. He or she would administer anti-fungal representatives, sometimes both topically to the eye and orally, depending on the severity of the ulceration. The diagnosis for excellent vision depends upon the level of infection.
Even if detected early and handled properly, some cases of corneal ulcers will require a cornea transplant (penetrating keratoplasty).
I had corneal ulcers when as a teen, and it was awful! My eye doctor has mentioned there are often eye issues that come along with UC, so there is a possibility this relates. My doc was in fact stunned I didn’t have more eye problems, given the seriousness of my UC. I do get the floaters a lot however, and have some minor damage from prednisone.