Duane syndrome impacts the eye muscles so that the capability to move the eye inward, external, or in both directions is restricted. In this article, you will learn more about the condition, its impact on everyday living, and when it needs treatment.
Likewise called Duane’s retraction syndrome, eye retraction syndrome, and Stilling-Turk-Duane syndrome, This uncommon disorder is caused by a “miswiring” of the medial and the lateral rectus muscles (the muscles that move the eyes) in the fetus in utero.
The exact cause is uncertain, but seems a mix of genetic and ecological elements. Direct sequencing of the CHN1 gene has identified mutations in the CHN1 gene, which are related to familial isolated Duane syndrome.
The breakdown is believed to take place in the third to 8th week of pregnancy, when eye muscles and cranial nerves are developing. This is because in addition to the eye muscles being affected, individuals with Duane syndrome may likewise lack the 6th cranial nerve, which is involved in eye movement.
Duane syndrome is normally discovered before the age of 10, and is more typical in girls than in young boys. Race and ethnic culture do not contribute in who is affected. The disorder might happen alone or in association with other syndromes, such as Okihiro syndrome, Wildervanck syndrome, Holt-Oram syndrome, Morning Glory syndrome, and Goldenhar syndrome.

About 30 percent of children with Duane syndrome might have a malformation of the skeleton, ears, eyes, kidneys, or nervous system.
In many children, just one eye is affected, frequently the left, although both eyes might be affected. Children with Duane syndrome may also have other eye problems:
- Disorders of other cranial nerves
- Nystagmus (an involuntary back-and-forth movement of the eyeball).
- Cataracts.
- Optic nerve abnormalities.
- Microphthalmos (unusually little eye).
- Hereditary crocodile tear syndrome (tearing while eating).
Symptoms of Duane Syndrome
Duane syndrome, first described by Alexander Duane and his associates, is identified by unusual movement in one or both eyes. An individual’s capability to move the eye external toward the ear (abduction) or inward towards the nose (adduction) might be limited.
Often, the eye movement is limited in both directions, or the individual is not able to move the eye at all. To compensate for the decline in eye movement, people with Duane syndrome turn their go to maintain binocular vision. In hindsight, this head turn or posture can typically be determined in photos.
There are three types of Duane syndrome, with type 1 being the most common:
- Type 1: Abduction is limited, however adduction is relatively normal.
- Type 2: Adduction is restricted, however kidnapping is fairly normal.
- Type 3: Ability to move the eye, or eyes, in both instructions (kidnapping and adduction) is limited.
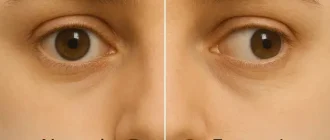
Often, when the eye approaches the nose, the eyeball pulls into the socket (this is called retraction). The limited eye motion might cause eyelid narrowing, and the affected eye might appear smaller than the other eye.
Likewise with particular eye motions, the eye might occasionally deviate upward or downward (called upshoot or downshoot).
Individuals with Duane syndrome may be more classified by their main gaze, depending upon where the eyes are when looking straight ahead. They might have:
- Esotropia (the affected eye is turned inward toward the nose).
- Exotropia (the affected eye is turned external towards the ear).
- Primary eye position (eyes are aligned).
Children with Duane syndrome who have actually misaligned eyes (strabismus) or minimized vision in the impacted eye needs to be examined by a pediatric eye professional early to avoid permanent vision disability or loss.
“The occurrence of Duane syndrome is 1% to 4% of strabismus patients. It is the most common type of congenital ocular aberrant innervation.” (British Journal of Ophthalmology, 2004).
Identifying Duane Syndrome
Duane syndrome is present at birth, but is frequently not acknowledged up until early youth, when abnormal head posture and strabismus emerge. Occasionally a child with Duane syndrome will have an affected family member. In these children, the condition has the tendency to affect both eyes.
A pediatric eye professional can detect Duane syndrome. Your child’s pediatrician or primary doctor might be able to find the condition during a regular workplace see. This would consist of an evaluation of your medical and family history and medical and vision examinations.
During the vision evaluation, your doctor will measure the degree of eye misalignment, test the variety of motion of both eyes, and identify whether the child is turning his/her head unusually in an effort to see better. The doctor will also search for any involved conditions.
No test for Duane syndrome is currently readily available. The medical diagnosis is based on medical findings. Genetic testing may be suggested for children with affected family members.
Although direct sequencing has actually recognized mutations on one gene, the chromosomal place of the proposed gene for this syndrome is currently unknown. Some research shows that more than one gene might be included.
When Is Treatment of Duane Syndrome Required?
Treatment is not always essential for people with Duane syndrome, if their symptoms do not interfere with daily living and they have no eye misalignment.
These people might have the ability to make up for minimal or lost eye movement with a slight turn of the head. In such circumstances, long-lasting tracking by their optometrist is often recommended.
For those with more severe symptoms, eye muscle surgery is normally required:.
“The significant indications for surgical correction in patients with Duane syndrome are an irregular head position of higher than 15 degrees and/or a substantial discrepancy in main [eye] position.” (British Journal of Ophthalmology, 2004).
There are several surgical options, consisting of ipsilateral rectus muscle economic downturn, vertical rectus muscle transposition, lateral posterior fixation stitches, synchronised medial and lateral rectus economic downturns, and surgery on the normal eye. The particular treatment or surgery is figured out by patient age, type of Duane syndrome, particular symptoms, household preference, and whether there are any related conditions.
The objective of treatment is to bring back satisfying eye alignment in the straight-ahead position, get rid of abnormal head posture, and avoid amblyopia. Surgery repositions the muscles, which permits better eye function, however it can not bring back eye function entirely. Still for the most parts, outcomes after surgery are reported to be good to exceptional.