Glaucoma refers to a group of related eye conditions that cause damage to the optic nerve that brings information from the eye to the brain. Glaucoma generally has couple of or no initial symptoms.
In many cases, glaucoma is associated with higher-than-normal pressure inside the eye — a condition called ocular hypertension. But it likewise can occur when intraocular pressure (IOP) is normal. If neglected or uncontrolled, glaucoma first causes peripheral vision loss and eventually can lead to loss of sight.
According to the American Academy of Ophthalmology, the most typical kind of glaucoma — called primary open-angle glaucoma — impacts an estimated 2.2 million people in the United States, which number is anticipated to increase to 3.3 million by 2020 as the U.S. population ages.
And due to the fact that a lot of cases of glaucoma have few or no early symptoms, about half of Americans with glaucoma do not know they have it.
Glaucoma is the second-leading reason for blindness in the United States (behind macular degeneration), and the second-leading cause of blindness around the world (behind cataracts).
Causes of Glaucoma
A current discovery from scientists is supplying some new insights into what causes glaucoma.
Formerly, the permanent eye disease was related to raised eye pressure and vision loss. The cause and effect factors were never clear, even for professionals in the field.
The new researches suggest vision loss in individuals with glaucoma is caused by an immune action to early exposure to bacteria, which can raise eye pressure and trigger heat shock proteins.
These proteins are developed to react to stress factors.
Memory T cells then spot the heat shock proteins and wrongly see the nerve cells in the retina as foreign bodies and attack.
The autoimmune ambush causes vision disruptions, vomiting, and extreme eye pain.
The fact is, eye pressure is just a threat factor, which means only a small portion of people who have elevated ocular, or eye pressure, really develop glaucoma. Our study actually reveals that the elevated eye pressure does not naturally result in glaucoma.
The research study opens chances for targeted treatment alternatives and possibly even a treatment.
Targeted manipulation of the immune response in the eye will help remove the disease.
Types Of Glaucoma
The two significant classifications of glaucoma are open-angle glaucoma (OAG) and narrow angle glaucoma. The “angle” in both cases describes the drainage angle inside the eye that manages the outflow of the watery fluid (aqueous) that is continually being produced inside the eye.
If the aqueous can access the drain angle, the glaucoma is called open angle glaucoma. If the drainage angle is blocked and the liquid can not reach it, the glaucoma is called narrow angle glaucoma.
Types of OAG include: primary open angle glaucoma (POAG), normal-tension glaucoma (NTG), pigmentary glaucoma, pseudoexfoliation glaucoma, secondary glaucoma and hereditary glaucoma.
Variations of narrow angle glaucoma consist of consist of severe angle closure glaucoma, chronic angle closure glaucoma, and neovascular glaucoma.
- Main open-angle glaucoma. This typical type of glaucoma gradually minimizes your peripheral vision without other symptoms. By the time you observe it, long-term damage already has occurred.
If your IOP remains high, the damage triggered by POAG can advance till tunnel vision develops, and you will be able to see just objects that are straight ahead. Eventually, all vision can be lost, triggering loss of sight.
- Intense angle-closure glaucoma. Likewise called narrow-angle glaucoma, intense angle-closure glaucoma produces sudden symptoms such as eye pain, headaches, halos around lights, dilated students, vision loss, red eyes, nausea and vomiting.
These signs make up a medical emergency situation. The attack may last for a couple of hours, then return once again for another round, or it may be constant without relief. Each attack can cause progressively more vision loss.
- Normal-tension glaucoma. Like POAG, normal-tension glaucoma (likewise called normal-pressure glaucoma, low-tension glaucoma or low-pressure glaucoma) is a kind of open-angle glaucoma that can cause visual field loss due to optic nerve damage. But in normal-tension glaucoma, the eye’s IOP stays in the normal range.
Likewise, pain is not likely and long-term damage to the eye’s optic nerve may not be noticed till symptoms such as one-track mind happen.
The reason for normal-tension glaucoma is unknowned. But numerous medical professionals think it belongs to poor blood flow to the optic nerve. Normal-tension glaucoma is more typical in those who are Japanese, are female and/or have a history of vascular disease.
- Pigmentary glaucoma. This rare kind of glaucoma is caused by clogging of the drainage angle of the eye by pigment that has actually broken out from the iris, decreasing the rate of aqueous outflow from the eye. In time, an inflammatory reaction to the blocked angle harms the drainage system.
You are unlikely to notice any symptoms with pigmentary glaucoma, though some pain and blurry vision may take place after workout. Pigmentary glaucoma most regularly impacts white males in their mid-30s to mid-40s.
- Secondary glaucoma. Symptoms of chronic glaucoma following an eye injury might show secondary glaucoma, which also may establish with existence of eye infection, swelling, a tumor or enlargement of the lens due to a cataract.
- Genetic glaucoma. This acquired type of glaucoma exists at birth, with 80 percent of cases detected by age one. These children are born with narrow angles or some other defect in the drain system of the eye.
It’s difficult to spot signs of genetic glaucoma, due to the fact that children are too young to comprehend what is taking place to them. If you observe a cloudy, white, hazy, bigger or protruding eye in your child, consult your eye doctor. Genetic glaucoma normally occurs more in kids than in girls.
Who Is At Risk to Get Glaucoma?
Open-angle glaucoma is 3 times most likely to affect African-Americans, compared with non-Hispanic whites in the United States, and loss of sight from glaucoma is at least six times more widespread among African-Americans than non-Hispanic whites.

The “risk groups” for glaucoma include:
- People over the age of 60-70 who don’t even present eye complaints;
- People over 40 years of age who have:
- intraocular pressure is at the upper limit of normal;
- the difference between the intraocular pressure of the right and left eyes is more than 5 mm Hg;
- the difference between the intraocular pressure measured in the morning and in the evening is more than 5 mm Hg;
- people with high myopia after the age of 40-50, with high hyperopia (especially women after 50);
- people with elevated intraocular pressure, regardless of age;
- people with low (relative to age norm) blood pressure;
- people with diabetes, endocrine, nervous, and cardiovascular diseases;
- People who have had eye injuries, inflammatory diseases (uveitis, iridocyclitis, etc.) of the eye, eye surgery;
- relatives (including distant relatives) of glaucoma patients with similar features of the eye structure;
- people undergoing long-term treatment with hormones.
Glaucoma can occur at any age, but the disease most often develops in older people.
Studies also suggest open-angle glaucoma affects Hispanics and Latinos at comparable rates to African-Americans.
And in a study released in 2014 that compared the frequency of two types of open-angle glaucoma– main open-angle glaucoma (POAG) and normal-tension glaucoma (NTG)– amongst Filipino and white Americans age 40 and older, researchers found Filipino Americans were more commonly detected with both types of open-angle glaucoma than white Americans (11.9 vs 8.2 percent for POAG; 6.8 vs. 2.5 percent for NTG).
Also, amongst Filipino Americans detected with open-angle glaucoma, 46.7 percent had the normal-tension range, whereas only 26.8 percent of whites with open-angle glaucoma had NTG, which can be more challenging to treat than POAG.
Glaucoma Symptoms
Glaucoma typically is called the “quiet burglar of sight,” because many types usually cause no pain and produce no symptoms until visible vision loss occurs.
For this factor, glaucoma typically advances undetected until the optic nerve already has been irreversibly damaged, with varying degrees of long-term vision loss.
But with acute angle-closure glaucoma, symptoms that occur all of a sudden can consist of blurred vision, halos around lights, intense eye pain, queasiness and vomiting. If you have these symptoms, make sure you see an eye care practitioner or go to the emergency room immediately so steps can be taken to prevent long-term vision loss.
Diagnosis, Screening And Tests For Glaucoma
Depending on individual indications, our patients may be offered the following methods of glaucoma diagnosis:
- Tonometry. A diagnostic procedure necessary to assess the risk of glaucoma, which involves measuring intraocular pressure (IOP). Tonometry is also widely used by ophthalmologists to monitor IOP status over time.
- Perimetry. Examination of the visual field, one of the methods of diagnosing glaucoma, partial optic atrophy.
- Gonioscopy. In the course of gonioscopy the study of the anterior chamber of the eyeball is performed, and the type of glaucoma (closed-angle or open-angle) is determined.
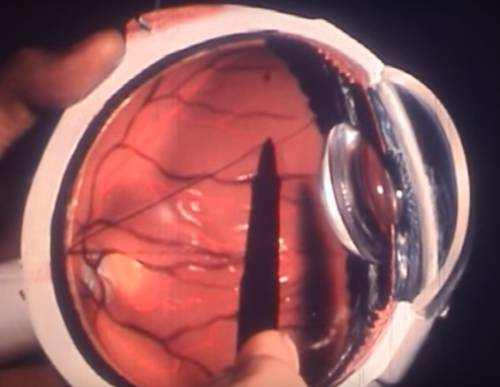
- Biomicroscopy. A procedure to study different parts of the eye with a special ophthalmic microscope, the slit lamp. During biomicroscopy the conjunctiva, cornea, iris, vitreous body, lens, central sections of the eye fundus are examined in detail.
- Optical coherence tomography. Today is the most up-to-date method of studying different structures of the visual system. OCT allows making two or three dimensional images of the retina and optic nerve disc.
- Pachymetry. A diagnostic tool to measure the size of the lens – in some cases glaucoma develops due to its abnormal parameters.
During routine eye tests, a tonometer is used to determine your intraocular pressure, or IOP. Your eye typically is numbed with eye drops, and a little probe carefully rests against your eye’s surface. Other tonometers send out a puff of air onto your eye’s surface area.
An unusually high IOP reading indicates a problem with the quantity of fluid (aqueous humor) in the eye. Either the eye is producing too much fluid, or it’s not draining appropriately.
Generally, IOP needs to be below 21 mmHg (millimeters of mercury) – a system of measurement based on how much force is exerted within a certain defined area.
If your IOP is higher than 30 mmHg, your risk of vision loss from glaucoma is 40 times greater than someone with intraocular pressure of 15 mmHg or lower. This is why glaucoma treatments such as eye drops are developed to keep IOP low.
Other methods of keeping an eye on glaucoma involve the use of advanced imaging technology — such as scanning laser polarimetry (SLP), optical coherence tomography (OCT) and confocal scanning laser ophthalmoscopy — to develop baseline images and measurements of the eye’s optic nerve and internal structures.
Then, at defined periods, extra images and measurements are taken to make certain no modifications have actually taken place in time that might show progressive glaucoma damage.
Visual field testing is a way for your eye doctor to figure out if you are experiencing vision loss from glaucoma. Visual field testing involves staring directly ahead into a device and clicking a button when you discover a blinking light in your peripheral vision. The visual field test may be duplicated at regular periods to make sure you are not establishing blind spots from damage to the optic nerve or to identify the level or development of vision loss from glaucoma.
Gonioscopy likewise might be performed to make sure the aqueous humor (or “aqueous”) can drain pipes freely from the eye. In gonioscopy, special lenses are used with a biomicroscope to allow your eye doctor to see the structure inside the eye (called the drainage angle) that controls the outflow of liquid and therefore affects intraocular pressure. Ultrasound biomicroscopy is another technique that may be used to assess the drain angle.
Glaucoma Treatments
Treatment can involve glaucoma surgery, lasers or medication, depending on the severity. Eye drops with medication focused on decreasing IOP typically are attempted first to control glaucoma.
Because glaucoma often is painless, people may end up being reckless about strict use of eye drops that can control eye pressure and help prevent irreversible eye damage.
In truth, non-compliance with a program of prescribed glaucoma medication is a major factor for blindness caused by glaucoma.
If you discover that the eye drops you are using for glaucoma are uneasy or inconvenient, never ever discontinue them without first consulting your optometrist about a possible option therapy.
Conservative (using medications) treatment
Treatment with the latest generation of anti-glaucoma medications is primarily aimed at reducing intraocular fluid production and improving its outflow, and the IOP is normalized.
But drug treatment is often effective only at the early stages of glaucoma. Besides, conservative therapy is not suitable for all patients due to the possible side effects of medications, vascular diseases, bronchial asthma and some endocrine pathologies. In addition, any prolonged drug therapy loses effectiveness over time. Therefore, surgical intervention is the most effective method of glaucoma treatment.
Laser treatment
Conventional surgical procedures as well as laser surgeries are performed for closed-angle glaucoma.
- Laser iridotomy (IAG). An intervention that creates a microscopic hole or several holes near the iris to lower the IOP. Statistically, after a laser iridotomy, 90% of patients have normalized intraocular pressure.
- Selective laser trabeculoplasty. This procedure is aimed at normalizing the intraocular pressure. For this purpose, the outflow blockage of the intraocular fluid is removed during the surgery.
If glaucoma is caused by the fact that the crystalline lens does not match the size of the eye, ophthalmic surgeons use the method of removing the crystalline lens with simultaneous implantation of an intraocular lens. As a result, the natural circulation of fluid in the eye is restored, which prevents vision loss.
The advantages of laser treatment for glaucoma are:
- restoration of the outflow of intraocular fluid from the eye through natural pathways;
- High efficiency of reducing intraocular pressure;
- Minimal risk of complications;
- Laser interventions are painless and are performed under local anesthesia with pain-relieving drops;
- laser treatment is short in duration and performed on an outpatient basis;
- Short and short period of recovery (rehabilitation).
Laser glaucoma treatment is most effective at early stages of the disease.
Depending on the type of glaucoma – open-angle or closed-angle, the nature of changes in the drainage apparatus of the eye, different types of laser interventions (surgeries) are applied.
Simultaneous treatment of glaucoma and cataracts
Specialized clinics perform one-stage surgical treatment of cataract and glaucoma. This procedure maintains eye health and restores visual acuity without the need for additional surgical interventions.
In cases where cataract and secondary glaucoma are combined, the patient is offered ultrasonic phacoemulsification of cataract with implantation of intraocular lens, artificial lens, and the intraocular pressure returns to normal. Ultrasonic phacoemulsification effectively treats cataract and stops further development of glaucoma.
If a cataract develops in the presence of existing glaucoma two surgeries are performed at the same time: ultrasonic phacoemulsification of the cataract and an anti-glaucoma surgery which if necessary is performed using special drains.
Antiglaucoma surgery restores the natural balance of fluid in the eye and normalizes the intraocular pressure. Ultrasonic phacoemulsification allows to get rid of cataract.
Treatment of glaucoma in the elderly
Many elderly people connect deterioration of vision with age and turn to the doctor when they cannot see properly. Open angle glaucoma, which is the type of pathology most frequently encountered in elderly patients, develops slowly, but may be detected at an early stage and treated to preserve vision.
Glaucoma can be suspected by the following symptoms: shadows before the eyes, frequent migraines, halos in front of the eyes, pressure on the eyeballs, narrowing of the visual fields.
In 90% of cases elderly patients have open angle glaucoma. In this case an anti-glaucoma surgery becomes an effective method of treatment. Such surgery restores the natural balance of fluid in the eye.
Glaucoma Prevention
Can you decrease your risk for glaucoma? According to a current European study, workout might work for some people.
Scientists in the U.K. found that greater levels of physical exercise appear to provide a long-lasting benefit of minimizing the occurrence of low ocular perfusion pressure (OPP), an essential risk factor for glaucoma. OPP is a mathematical value that is computed using a person’s intraocular pressure and his or her blood pressure.
The outcomes revealed that research study individuals who engaged in moderate exercise around 15 years prior to the study had a 25 percent decreased risk of low OPP that could cause glaucoma.
“It appears that OPP is mostly figured out by cardiovascular fitness,” said research study author Paul J. Foster, MD, PhD, of the University College London Institute of Ophthalmology. “We can not discuss the cause, however there is definitely an association in between an inactive lifestyle and factors which increase glaucoma risk.”
Maintaining an active lifestyle seems a reliable method for people to lower their risk of glaucoma and lots of other serious health problems, Dr. Foster concluded.
In addition to regular workout and an active lifestyle, you likewise can minimize your risk for glaucoma by not cigarette smoking, preserving a healthy weight, and consuming a different and healthy diet.
What Else You Should Know about Glaucoma?
Q. What are acceptable eye pressures and at what ages?
A. Intraocular pressure works differently in different individuals, and there is not one pressure level that works for everyone. When your doctor performs a thorough eye assessment, that s/he is likely recognizing a target pressure measurement that s/he believes would be “normal” for your specific condition, implying it would hopefully prevent additional optic nerve damage from taking place if you could support your pressure at this target level. It would be very appropriate for you to ask your treating physician what this target number is so that you can analyze and comprehend how your eyes are doing each time you go to the physician for an eye examination. To put intraocular pressure measurements in point of view, the national average pressure measurement in the U.S. is between 14 and 16, and average population pressures approximately 21 might be within a reasonable range. There are also many other personal qualities and hereditary problems, such as race, family history and corneal thinness just among others, that should be thought about when a physician examines your examination outcomes and figures out whether your present condition can be harming to your optic nerve. We motivate you to ask concerns and regularly interact with your medical professional so that you can be an active and understanding individual in your treatment plan. If you continue to have concerns about the right course of treatment for your glaucoma, think about seeking a 2nd or perhaps third opinion from another physician.
Q. I have cataracts, can my glaucoma be dealt with, and how?
A. Cataracts and glaucoma are two different issues. Cataracts can be treated by having them removed with a reasonably benign surgery. Frequently, however, a combined procedure can be performed at the time of cataract extraction, consequently, ideally getting glaucoma under control. Remember, the glaucoma is not cured, just managed.
Q. Do some people with glaucoma produce excessive fluid and likewise have a drainage problem?
A. The fluid is continuously produced within the eye by a small gland called the ciliary body. This clear fluid, referred to as aqueous humor, supplies the internal structures of the eye with nutrients and oxygen. The fluid then exits the eye through the drain angle, which is called the trabecular meshwork. Increased resistance within the trabecular meshwork decreases the rate of flow throughout it and causes a buildup of fluid within the eye, leading to raised eye pressure. This is invariably a result of bad drainage function, rather than a boost in liquid humor production by the ciliary body.
Raised eye pressure in glaucoma happens because the rate of fluid production goes beyond the eye’s capability to drain it. The degree of this resistance to outflow differs from individual to private. This scenario is comparable to your cooking area sink. The faucet is always on, and water goes down the drain. Envision that you put coffee grinds into the sink. What takes place? The water level gradually increases and after that, overruns. In the eye, the fluid can’t overflow, so the pressure goes up. Glaucoma medications lower intraocular pressure by either decreasing fluid production (denying the faucet) or increasing fluid outflow from the eye (enhancing the function of the drain).
Q. What is Pre-Glaucoma?
A. This is another method of stating that you are a glaucoma suspect. A glaucoma suspect is somebody who might have glaucoma; however, it’s too early to tell. This term includes patients with ocular high blood pressure (persons with elevated intraocular pressure but no noticeable disc or visual field damage) and patients with big cup/disc ratios and normal visual fields who might or might not have early normal-tension glaucoma. Since you have been detected as a glaucoma suspect, you must see your eye care professional frequently to monitor your condition so that you do not experience any loss of vision.
Q. What is the difference between cataracts and glaucoma?
A. The optical system of the eye allows us to see. When the light goes into the eye, it is focused by the lens onto the retina, which views the image, much in the very same way an electronic camera lens focuses light onto the film to record a picture. As we age, the generally clear lens starts to thicken and slowly ends up being tarnished. This condition is called a cataract. This results in a loss of vision and takes place at various rates in various individuals. Vision loss in glaucoma occurs since of damage to the optic nerve, which links the eye to the brain. Because of its similarity to the nerve cells (called neurons) of the brain, once it is injured, it can not be fixed. The loss of afferent neuron is irreversible.
Cataracts and glaucoma might take place together in the exact same individual. For the majority of people, these two disease procedures are different and unique and might progress at different rates. It is essential to bear in mind that a cataract is a reversible type of vision loss and that glaucoma is not. Irreversible loss of vision from glaucoma, nevertheless, can be prevented in most people by early detection and careful follow-up examinations to detect early signs that the eye is being harmed, followed by proper, timely intervention must these signs develop.
Q. Can an individual who has had glaucoma and cataract surgery wear contacts?
A. Most individuals who undergo cataract surgery no longer required to use contact lenses due to the fact that their nearsightedness or farsightedness is usually corrected when the lens implant is put. This correction of vision should be talked about before surgery so that the client and the medical professional are pleased with the postoperative visual results. Although patients who undergo cataract surgery alone may normally have the ability to tolerate contact lenses after surgery, some people who also go through glaucoma surgery might not be able to use contact lenses after surgery because of changes which take place on the surface of the eye after glaucoma surgery. The use of contact lenses after eye surgery should be discussed with your medical professional both before and after the surgery.
Q. Is my blood pressure connected to my eye pressure (IOP)?
A. Blood pressure and eye pressure differ individually. Controlling blood pressure does not indicate IOP is controlled. But studies have shown that patients with high blood pressure have an increased danger for glaucoma.
The relationship of low blood pressure to glaucoma has been better developed. Chronic low blood pressure is a threat aspect of establishing progressive glaucoma damage. We now comprehend that in some kinds of glaucoma, there is a strong link between glaucoma and bad (reduced) blood flow to the optic nerve. Low blood pressure is strongly associated with normal-tension glaucoma– a type of glaucoma that occurs even though the pressure inside the eye is not raised.
Patients who are taking medication for hypertension might have their blood pressures dropping to very low levels during the hours they are sleeping. This decreases the quantity of blood circulation to the eye and optic nerve and might jeopardize the optic nerve. The function of blood circulation in optic nerve damage is the subject of continuous study.
Patients with any progressive glaucoma need to make sure their blood pressure is not dropping to very low levels while they sleep. Your ophthalmologist needs to know about all your medical conditions and the medications you are taking and needs to work with your other doctors to ensure everything is in synch.
Q. Is glaucoma hereditary?
A. Glaucoma is a group of disorders, a variety of which are triggered at least in part by genetics and the action of genes. Nevertheless, just a little percentage of genes that determine danger for glaucoma have been found, and many are still unidentified. Particular genes can affect the development and likely the progression of the disease.
Q. Are there gender-based risk factors for glaucoma?
A. A glaucoma is a group of related diseases that share a common endpoint: glaucomatous damage to the optic nerve. Research studies have certainly revealed that women are 3 to 5 times more likely to have angle-closure glaucoma, one kind of the disease. When it concerns main open-angle glaucoma (POAG), the most common form of the disease, research studies have not shown a conclusive gender predisposition.
As women outlive men around the world, and age is among the threat elements for glaucoma, it is expected that statistically more women have glaucoma than men. There is some proof that female sex hormonal agents might be protective of the optic nerve. It has actually also been hypothesized that with age, decreased estrogen may be associated with increased risk for POAG. However, the results of related research studies have to date been undetermined. Nevertheless, age remains the main threat factor for glaucoma, and tracking for the disease is specifically important. Everybody 40 or older must have a detailed dilated eye assessment every one and a half to 2 years. If you are 40 or older and have an extra danger factor, get checked annually.
Q. What type of doctor should I see about glaucoma?
A. Optometrists (ODs), eye doctors (MDs) and glaucoma specialists are all qualified eye care specialists who can provide comprehensive eye examinations.
Eye doctors can examine the eye to diagnose and treat vision problems and problems through non-surgical means, and prescribe glasses, contact lenses, and some kinds of medications.
Eye doctors have gotten graduate training in a medical school and then sub-specialized in the medical and surgical treatment of eye diseases and injuries. They see patients for regular eye care, do eye evaluations, prescribe medications, and carry out eye surgery.
Glaucoma Specialists are ophthalmologists who have finished additional post-residency fellowship training specific to glaucoma.