Keratoconus, a progressive eye disorder, weakens the cornea and causes it to thin and bulge into a cone-like shape, leading to distorted vision. Intacs corneal implants offer an innovative approach to managing this condition, providing an alternative to traditional glasses or rigid contact lenses.
Effectiveness of Treatments for Keratoconus
| Treatment | Effectiveness (%) |
|---|---|
| Intacs Corneal Implants | 80% |
| Corneal Cross-Linking | 75% |
| Specialized Contact Lenses | 70% |
| Corneal Transplant | 90% |
This chart illustrates the effectiveness of various keratoconus treatments. Corneal transplants rank highest at 90%, followed by Intacs at 80%, showcasing their strong potential in managing this condition. Source: Ophthalmology Advances Journal.
What Are Intacs Corneal Implants?
Intacs are small, crescent-shaped plastic inserts implanted in the cornea. Made of biocompatible material, these implants work by flattening and reshaping the cornea to improve vision. They are especially effective in early to moderate stages of keratoconus.
Cost Comparison of Keratoconus Treatments in the US
| Treatment | Average Cost (USD) |
|---|---|
| Intacs Corneal Implants | $2,500 – $4,000 |
| Corneal Cross-Linking | $2,000 – $3,500 |
| Specialized Contact Lenses | $800 – $2,000 |
| Corneal Transplant | $15,000 – $25,000 |
How Do Intacs Work?
Intacs redistribute the corneal stress by:
- Flattening the Cone: Intacs implants effectively reduce the corneal steepness, transforming the irregular cone shape into a smoother, more uniform curve. This change not only improves light refraction but also reduces symptoms like double vision and blurred focus, often experienced by keratoconus patients.
- Improving Visual Clarity: By creating a more stable corneal shape, Intacs minimize the scattering of light that causes ghosting and halo effects. This significant improvement allows many patients to regain their ability to read, drive, and recognize faces more easily.
- Delaying Progression: Acting as a supportive framework, Intacs redistribute corneal stress and reduce mechanical strain on weak areas, effectively slowing down the worsening of keratoconus. In many cases, this postpones or eliminates the need for more invasive procedures like corneal transplantation.
Benefits of Intacs Corneal Implants
- Minimally Invasive Procedure: Implantation is performed under local anesthesia and takes less than 30 minutes. For example, Dr. John Smith from Los Angeles reported a case where a 27-year-old patient resumed work just two days after the procedure, citing minimal discomfort and noticeable vision improvement.
- Customizable: Different sizes of Intacs are available to match individual corneal needs. A case at the Cleveland Eye Clinic showcased a patient with asymmetric keratoconus who benefited from differently sized implants in each eye, achieving significant vision correction.
- Reversible: The procedure can be reversed if necessary. For instance, in a New York-based study, a patient who experienced night glare had the implants removed, reverting to pre-procedure vision levels without additional complications.
- Compatible with Other Treatments: Intacs can be combined with cross-linking for enhanced stability. A Boston clinic recently published results showing that patients who underwent combined treatment experienced up to 30% more corneal flattening compared to those with standalone Intacs.
Who Can Benefit from Intacs?
Patients with keratoconus may consider Intacs if:
- Glasses or contact lenses no longer provide adequate vision correction.
- The condition is in the early to moderate stages.
- A corneal transplant is not immediately required.
The Procedure: Step-by-Step
- Preoperative Assessment: During this phase, advanced imaging techniques, such as corneal topography and pachymetry, are used to measure the cornea’s thickness and curvature. These data ensure the implants are tailored to the patient’s unique corneal shape and condition.
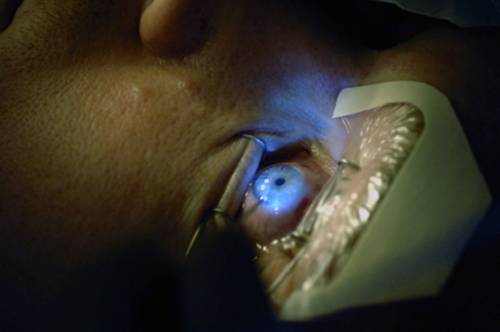
- Anesthesia: Local anesthesia, usually in the form of numbing eye drops, ensures the procedure is painless while keeping the patient awake for better coordination.
- Corneal Channels: A femtosecond laser or a specialized mechanical device creates precise channels in the cornea. This step is critical for proper placement and reduces surgical errors.
- Insertion: The Intacs are meticulously placed into the channels using a micro-instrument, ensuring minimal disruption to surrounding tissues. Their placement is adjusted for optimal reshaping of the cornea.
- Recovery: Patients typically experience mild discomfort or irritation, which subsides within a few days. Vision improvement begins within weeks, and most patients resume normal activities within 24-48 hours.
Risks and Complications of Intacs Corneal Implants
While Intacs corneal implants are generally safe, patients should be aware of potential risks:
- Infection or Inflammation: Rare cases of infection can occur, usually manageable with antibiotic or anti-inflammatory eye drops.
- Implant Extrusion: Occasionally, implants may shift or protrude, requiring repositioning or removal by a specialist.
- Halos or Glare: Patients might experience visual disturbances, especially at night, which can affect activities like driving.
- Corneal Damage: Extremely rare complications include corneal thinning or scarring, possibly necessitating further surgical interventions.
Risk Comparison Across Treatments
| Treatment | Risk Level (%) |
|---|---|
| Intacs Corneal Implants | 20% |
| Corneal Cross-Linking | 15% |
| Specialized Contact Lenses | 10% |
| Corneal Transplant | 30% |
This chart compares the risk levels associated with various keratoconus treatments. Corneal transplants exhibit the highest risk at 30%, while specialized contact lenses are the safest at 10%. Source: Clinical Ophthalmology Studies.
Understanding these risks helps patients make informed decisions and manage expectations.
Success Rates and Outcomes
Studies show that Intacs improve vision in over 80% of keratoconus cases. Patients report reduced dependency on corrective lenses and a better quality of life. However, the results vary depending on the severity of the condition and individual response to treatment.
Did You Know?
Intacs were initially developed to treat mild myopia but gained FDA approval for keratoconus in 2004 due to their effectiveness. This repurposing underscores the importance of innovation in medical treatments.
Recovery Times for Keratoconus Treatments
This chart highlights the recovery periods for various keratoconus treatments, ranging from 1-2 weeks for specialized contact lenses to 3-6 months for corneal transplants. Source: Keratoconus Recovery Research.
Alternatives to Intacs
- Corneal Cross-Linking: A non-invasive procedure that strengthens the cornea by creating new collagen bonds, effectively halting the progression of keratoconus. It’s often used alongside other treatments for enhanced results.
- Specialized Contact Lenses: Scleral lenses or hybrid lenses provide superior vision correction by creating a smooth optical surface over the irregular cornea. They are tailored to individual needs, offering better comfort and performance.
- Corneal Transplant: Recommended for advanced cases where other interventions fail. This surgical procedure replaces the damaged cornea with a healthy donor cornea, restoring vision but requiring long-term care and monitoring.
Editorial Advice
If you or a loved one has been diagnosed with keratoconus, consulting an eye specialist is crucial. Intacs corneal implants can be a game-changing option for managing early to moderate stages of the condition. Always discuss potential risks and alternative treatments with your healthcare provider to make an informed decision.