What is keratoconus? We will discuss the causes, diagnosis, and treatment methods in our article.
What is the disease
Keratoconus is a chronic disease of the cornea, in which it loses its ability to maintain its spherical shape, becomes thin, stretches, becomes cloudy and does not perform its natural functions. Today, this diagnosis is often found in doctors’ reports.
What are the dangers of keratoconus
Without treatment, the disease leads to a progressive decrease in visual acuity, loss of ability to work and disability of the patient, up to blindness.
Causes of keratoconus
This disorder was first described in detail in 1854, but so far there is no unequivocal medical opinion on its origin.
Depending on the causes, the disease may be primary or secondary.
Primary (congenital) keratoconus develops spontaneously, as if for no apparent reason. Why does the process of corneal changes start suddenly? Today medical science has no single answer – there are only many theories of the disease development. Let’s consider the most popular ones.
- Heredity. Science gives about 10% to this factor. Most often there is an autosomal dominant type of inheritance – when there is a genetic defect in at least one of the parents. Undeniable evidence of this theory is family cases of keratoconus, its frequent association with a number of hereditary diseases and syndromes, as well as established features of the course of keratoconus in monozygotic and dizygotic twins. According to statistics, keratoconus is more common in people of mongoloid race and southern nationalities (Azerbaijanis, Armenians, etc.)
- Natural and environmental conditions. The prevalence of keratoconus in the population of England is 3.3 per hundred thousand people, while in New Zealand, where people from the same country live, it is more than 20 per hundred thousand people. Such a tangible difference in similar genetic groups is related to changed climatic conditions – increased solar insolation. In countries with a colder climate (Finland, Denmark, Japan, and Russia), the incidence of keratoconus is much lower, and the forms of the disease are less aggressive.
- The environmental factor also plays a role. For example, keratoconus in highly industrialized mountainous regions of the Urals occurs much less frequently (one per 500 thousand people) than in steppe ecologically favorable regions (one per a hundred thousand people). And in 83% of cases children, teenagers and young people under 29 years old fall ill.
- Immunoallergic theory. About 30 years ago increased serum levels of immunoglobulin (Ig) class E, antibodies involved in immune response, were found in about 59% of patients with keratoconus. Today it is known for sure that people with keratoconus have disturbed immune homeostasis (protection of the organism from external factors), increased number of Ig M, C3 and C4 components of complement, enhanced defect of T-suppressors and increased number of Ig G, which lead to failure of autolerance (resistance of the organism) to their corneal antigens. But despite such data, the reliability of the relationship is contradictory and has not been confirmed in multicenter studies.
- Neurohumoral theory. The onset of keratoconus more often occurs during puberty. Many authors see the role of endocrine factors, imbalance of pituitary-diencephalic system, adiposogenital insufficiency, hyper- or hypothyroidism.
- The literature also covers the viral and metabolic theories, the descemetal membrane (corneal layer) pathology theory, and others. Their multifactorial nature indicates that there is still no unified and complete understanding of the cause of keratoconus.
Secondary (acquired) keratoconus develops as a consequence of corneal surgery, such as popular excimer laser vision correction and keratotomy. This is due to the decrease in biomechanical properties of the cornea when its flap is formed and the total thickness of the corneal stroma (basic substance) decreases during excimer laser ablation.
Information about corneal subsidence (keratectasia) after excimer laser surgery was published in 1998. It was mentioned in the article that 4% of all patients with secondary keratoconus after PRK (photorefractive keratectomy) and 96% were patients after laser LASIK correction.
In Russia, the risk of surgery-induced keratoconus is 1-5%. According to foreign authors, the incidence varies between 0.02 % and 0.6 %. Improved methods of examination of patients and equipment make it possible to minimize the risks of keratoconus disease today.
Keratoconus and pregnancy
Hormones increase fluid retention in the corneal stroma even in healthy women. This is why keratoconus may become more pronounced during pregnancy. The development of the child and the pregnancy itself are not affected by the disease, the delivery is also done naturally if there are no other pathology and complications.
Symptoms of keratoconus
Typically, keratoconus develops in adolescents at 13-16 years of age. There are also cases of earlier (8-12 years) and later (20-30 years) onset.
Symptoms in children
The age at which the disease first appears depends on the progression rate of keratoconus: the younger the patient, the more pronounced the symptoms – changes in the cornea are faster and more severe. It is generally believed that the disease is most active in the first 5-10 years, after which the progression of the disease usually stops or slows down considerably. Thus, in people under the age of 30, keratoconus progresses in 80% of cases and in people older than 30 – only in 20% of cases.
Visual impairment
Often the first complaint of people with keratoconus is decreased vision, inability to improve visual acuity with the usual glasses or lenses, and frequent changes of glasses. Patients may also notice glare, flashes, distortion of objects, foggy images, redness, and dry eyes.
Further symptoms can be recognized by the doctor during the examination of the patient. They depend on the degree of keratoconus development:
- Astigmatism – the disease impairs the eye’s ability to focus light rays on the retina, increases pre-existing astigmatism, and increases the corneal refractive power over 45-46 dptr;
- thinning of the stroma (basic substance) of the cornea in the center, conical bulging forward;
- at corneal microscopy – cracks in the descemetal membrane (Vogt’s striae);
- superficial and then deep stromal scarring;
- in the terminal (final) stages – protrusion of the lower eyelid when looking downward (Munson’s symptom), ring-shaped deposition of gland in the epithelial layer around the cone (Kayser-Fleischer ring).
Pathogenesis of keratoconus

Keratoconus is a complex disease with a rather complex pathogenesis. Although today it is considered a “noninflammatory pathology”, numerous modern studies prove that inflammatory factors are actively involved in the development of keratoconus. Most studies have found increased levels of matrix metalloproteinase-9 (MMP-9) and pro-inflammatory immune system molecules – interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) in the tears of patients with keratoconus.
The cornea is transparent, and for a reason. Collagen, which is its main component, is not homogeneous. Different structural parts of the cornea are represented by different types of collagen. It is the ratio of collagen fibers that makes the cornea transparent.
In keratoconus the ratio of collagen fibers is disturbed: the total amount of collagen as well as collagen types I and III is reduced. Corneal deformation and clouding are also affected by changes in collagen fibrils orientation, which leads to their reorganization.
Stroma (basic substance) of cornea is represented mainly by collagen fibers immersed in extracellular glycoprotein matrix, which performs a function of connective tissue. Therefore, quantitative and qualitative changes occurring in abnormal development of connective tissue (dysplasia) affect its biomechanical properties as well.
| Stage of keratoconus | Clinical and morphological manifestations |
|---|---|
| I | ⠀-⠀astigmatism not exceeding 5 Dpt. ⠀-⠀keratometry (corneal curvature) up to 48dpts ⠀-⠀absence of corneal opacity ⠀-⠀Visual acuity 0.5-1.0 |
| II | ⠀-⠀appearance of Vogt lines ⠀-⠀astigmatism 5-8 Dpt. ⠀-⠀keratometry up to 53dpts ⠀-⠀pachymetry (corneal thickness) up to 400 μm ⠀-⠀absence of corneal opacities ⠀-⠀Visual acuity 0.1-0.4 |
| III | ⠀-⠀astigmatism up to 8-10 Dpt. ⠀-⠀Ceratometry over 53 Dpts ⠀-⠀pachymetry 300-400 μm ⠀-⠀absence of corneal opacities ⠀-⠀Visual acuity up to 0.09 |
| IV | ⠀-⠀clinical refraction not determined ⠀-⠀pachymetry less than 300 μm ⠀-⠀there is a central corneal opacity ⠀-⠀visual acuity 0.02 ⠀-⠀keratometry more than 55 dptr |
Four stages of keratoconus are also distinguished by biomicroscopy.
| Signs detected on examination | Stage I | Stage II | Stage III | Stage IV |
|---|---|---|---|---|
| Stromal rarefaction | + | |||
| Enhanced nerve imaging | + | + | + | +/- |
| Clouding of the stroma and descemetal membrane | + | |||
| Keratoconus lines | + | +/- | +/- | |
| Clouding of the bowmen’s membrane | + | + |
Complications of keratoconus
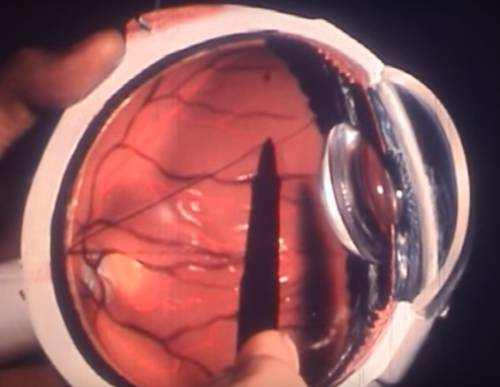
Acute keratoconus (corneal hydrocele) is a frequent and severe complication of a chronic process. It occurs due to rupture of the descemetal membrane.
Symptoms of acute keratoconus
Appears as a sharp decrease in visual acuity and a pronounced corneal syndrome – photophobia, burning and eye irritation.
There is no unified opinion on the tactics of acute condition management. Some authors think that no specific treatment is required since the condition will resolve itself. Others suggest that medical treatment or an active surgical approach is necessary: injection of autologous blood into the anterior chamber of the eye, bandaging of the cornea and even variants of keratoplasty – corneal transplantation.
In case of untreated acute keratoconus, corneal edema spontaneously resolves within 4-5 months. After the acute process is over, the cornea flattens slightly as a result of clouding formation and local closure of the descemetal membrane rupture zone.
Spontaneous corneal rupture (perforation) as a complication is quite rare. As a rule, it is observed in patients with extremely advanced keratoconus, although rare cases of perforation at the initial stages of the disease are described in the literature. The authors point out pregnancy, long-term local treatment with corticosteroids and ocular trauma as aggravating factors.
Diagnosis of keratoconus
First of all, visual acuity and autorefractometry – a detailed examination of the cornea of the eye – are checked. Autorefractometry test marks, such as rings, can be used to judge corneal deformity. If the cornea is cone-shaped, one ring takes the shape of an irregular oval, and the axes of the two rings do not match.
Using an autorefractometer or keratometer, you may find that the radius of curvature of the cornea has decreased and the keratometric data is irregularly increased. When keratoconus is more pronounced, it is not possible to obtain a test result. This is due to a high degree of astigmatism (corneal curvature) beyond the scope of measurement, or corneal opacity.
When performing skeascopy, an assessment of the eye’s ability to refract light, the “oil spot symptom” will be noticeable.
Corneal biomicroscopy, a check on the structure of the eye, is mandatory. It helps to see changes in the cornea: thinning or clouding of stroma, increased visualization of corneal nerves, clouding of descemetal membrane, conic shape, keratoconus lines, clouding of bowden membrane, etc.
Keratotopographer helps to reliably detect keratoconus even at its initial stage. It visualizes the entire cornea: corneal radius and thickness, anterior and posterior surface, asymmetries. The keratotopogram diagnoses irregular (irregular) astigmatism on the keratometric chart, elevation (elevation) of the posterior surface, thinning of the central corneal thickness. Often thinning areas are shown in red, and even the most inexperienced physician will be able to suspect pathology.
Anterior OCT – keratotomography – is also performed. It also visualizes corneal pathology, helps to monitor the disease dynamically, and even assess the presence of latent keratoconus, a non-progressive anomaly of the posterior corneal surface.
Laboratory diagnosis is not required.
Treatment of keratoconus
There is still no unified algorithm for the management of patients with keratoconus. Current literature presents treatment methods that focus on the stage of the disease.
The main task of a specialist, who has made a diagnosis of keratoconus, is to correctly inform the patient about the choice of treatment and rehabilitation methods.
Treatment of keratoconus at the initial stage
In the initial stage of keratoconus either contact or spectacle correction is performed, and in case of more severe keratoconus contact eye correction (scleral or rigid corneal lenses) or penetrating/layer keratoplasty is performed.
What are the treatment methods for keratoconus in contemporary ophthalmology?
Crosslinking
Cross linking is a treatment of keratoconus with the use of ultraviolet light and riboflavin (a special vitamin). Theo Seiler came up with this new method in 1997 and in 2003 the first clinical trials were published. Since then corneal cross-linking has entered clinical practice and has been widely used for more than 10 years in different European countries and more than five years worldwide. However, permission to perform the procedure in the U.S. was only granted in 2016.
The method is based on strengthening the biomechanical properties of the cornea – collagen fibers, connections between them, as well as their spatial structural arrangement. “Cross-linking” by ultraviolet light under the action of a sensitizer – 0.1 % riboflavin dissolved in 20 % dextran – inhibits metabolic processes in the stromal collagen, thereby increasing the biomechanical stability of the cornea.
Many different corneal cross-linking techniques have been developed. There are still numerous studies on the effectiveness of the techniques and the percentage of riboflavin used.
Crosslinking procedure is minimally traumatic, is performed under local anesthesia and is usually uncomfortable only in the first few days after the intervention. After treatment patients note an increase in visual acuity.
In 95% of cases cross linking stops keratoconus progression. Percentage of surgical risk is about 1% (infection, scarring, slow healing, etc.).
Cross-linking is performed even in adolescence, but its efficiency is higher in the early stages of the disease. In case of advanced keratoconus it is impossible to perform the procedure.
Corneal segment implantation
This method of treatment presupposes the strengthening of the cornea side, opposite to the apex of the stretching, with the help of special segments – rings. The introduction of such segments into the cornea improves visual functions (for instance, improves visual acuity), but does not solve the problem of keratoconus progression. Another disadvantage is the economic factor: the operation is quite expensive.
Segment implantation surgery is not technically complicated. Obligatory conditions for implantation are transparency of the central corneal zone and sufficient central thickness.
This method of treatment is indicated in the early refractive stages. Other advantages of implantation include:
- No risk of rejection;
- flattening of the cornea without invading its central zone;
- Significant persistent reduction in refraction;
- Reversibility of the procedure: in case of complications the segments are removed, preserving the ophthalmometric characteristics which were present before the surgery.
Keratoplasty
There are two variants of keratoplasty – layer-by-layer and through corneal transplantation.
The apotheosis of the battle for vision remains the end-to-end keratoplasty. Despite the use of a femtosecond laser, it is a high-risk operation. Its success depends on the patient’s age and condition.
Despite the widespread use of keratoplasty in the treatment of keratoconus, this surgery has disadvantages:
- The risk of graft rejection and the limited “life” of the graft;
- residual postoperative myopia and astigmatism;
- Long-term risks of infections;
- problems with donor material;
- high cost of the surgery.
Another unpleasant disadvantage of keratoplasty is the formation of new blood vessels in the cornea. In the absence of vessels in cornea the immune system has no direct access to its upper layer. In this case all immune processes are slow and gentle. When vessels appear, the immune system reacts sharply to the graft.
But probably the biggest disappointment of patients after keratoplasty is low visual acuity. This condition is associated with surgical astigmatism, which is almost impossible to avoid. According to Boston professor Perry Rosenthal, over 40% of patients after keratoplasty use correction, and their visual acuity averages 20/50 (0.4).
Deep layer-by-layer keratoplasty for keratoconus is just entering surgical practice. Its significant difference from penetrating keratoplasty is surgical correction of keratoconus with preservation of patient’s corneal endothelium. This reduces the risk of graft rejection.
Optical correction
The progression of keratoconus is a good reason to consult a surgeon about surgical intervention: cross linking or stromal segment implantation. But if there is no progression or if it is questionable, surgery is not justified. So what to do? To choose an adequate optical correction and to be observed dynamically.
There are several types of contact correction:
- soft individual lenses for keratoconus (several options);
- Hybrid lenses (a hybrid of soft and rigid lens);
- rigid gas-permeable corneal lenses and rigid corneoscleral lenses;
- rigid gas-permeable scleral lenses.
One popular way to compensate for visual acuity is with gas-permeable rigid lenses. They fit closely to the outside of the eye, smooth out any imperfections of the cornea and form the most correct optical surface.
Scleral gas-permeable lenses are quite specific. They rest on the sclera, and do not come into contact with the cornea and eyelids. They have a stable fit during the day, provide comfort and high visual acuity. Such lenses change the geometry of the cornea through the authentic tear film and fluid which allows to compensate the irregular astigmatism.
Optical correction can be used in combination with surgery: lens fitting after intrastromal segmentation or corneal transplantation. It allows patients to see the world in a better way.
Medication treatment
There are no medications to stop the development of keratoconus. Because of the irregular shape of the cornea and its thinning, patients suffer from dry eye syndrome. Tear substitutes (structural tear preparations) can improve the state of the anterior cornea surface.
Home remedies
It is not only useless, but also dangerous to use remedies of folk medicine. Without adequate treatment keratoconus results in decreased visual acuity up to blindness. Therefore, if keratoconus develops, it is necessary to consult a doctor who will choose the optimal method of treatment.
Prognosis. Prevention
To date, the disease is chronic in nature, and full recovery of the patient has not yet been achieved. However, modern methods of treatment and rehabilitation help to maintain a high quality of visual functions in patients with keratoconus at various stages.
Untreated progressive decrease in visual acuity can lead to disability and disability of the patient, up to blindness and the need for nursing care.
For people with keratoconus it is recommended a dynamic monitoring with control of keratotopograms in 4, 6, 12 months with a choice of the treatment tactics if necessary.
Currently, only secondary keratoconus prophylaxis is possible. It includes:
- Qualitative selection of patients for excimer laser surgery with posterior surface keratotopograms;
- If an increased risk is detected, a safer surgical method of excimer laser correction or active monitoring before the intervention (monitoring of corneal indices) is chosen for the patient;
- dynamic monitoring of patients who have undergone excimer laser treatment.