Meibomian Gland Dysfunction (MGD) might not be the catchiest name, but if you’ve ever struggled with gritty, irritated eyes, it’s time to learn about it. Often overlooked and underdiagnosed, MGD affects millions globally, leaving people wondering why their eyes feel dry, tired, and irritated. Let’s dive deep into the facts, statistics, and insights from ophthalmologists that will help you understand what MGD is and why you need to pay attention to it.
What is Meibomian Gland Dysfunction?
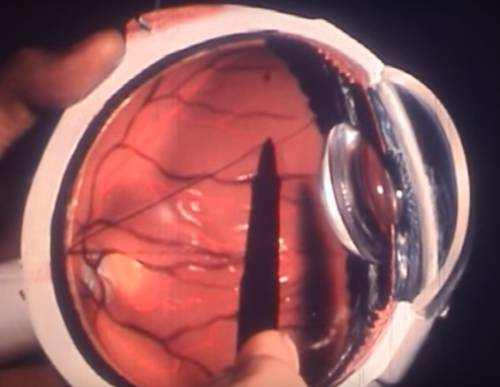
MGD is a condition where the meibomian glands in the eyelids become blocked or dysfunctional, leading to inadequate oil secretion into the tear film. These glands, numbering about 25-40 per eyelid, play a crucial role in maintaining a healthy tear film by releasing oil that prevents tears from evaporating too quickly. When these glands stop working properly, the tear film destabilizes, leading to dry eye symptoms.
How Common is MGD? The Numbers Speak for Themselves
MGD is extremely common, especially as we age. Studies suggest that up to 86% of individuals with dry eye syndrome actually suffer from MGD. To put it in perspective, one comprehensive study found that about 50-70% of adults over the age of 50 have some form of meibomian gland dysfunction. MGD is also strongly associated with the use of contact lenses, with 20-30% of long-term contact lens users developing meibomian gland issues.
Why Do the Meibomian Glands Malfunction?
The causes behind MGD are varied, and it’s not always easy to pinpoint exactly why the glands stop working. Age is a major factor, as gland function tends to decline with time. Other significant contributors include:
- Screen Time and Blink Patterns: Spending hours staring at a screen reduces blink frequency. Blinking is vital for stimulating oil release, and fewer blinks mean less oil is expressed, leading to blocked glands.
- Hormonal Changes: Especially in women, hormonal changes related to menopause can impact gland function. Low androgen levels are linked to a higher risk of MGD.
- Environmental Stressors: Exposure to dry, windy, or air-conditioned environments can exacerbate MGD, especially in climates that cause tears to evaporate faster.
Expert Insights on Diagnosis and Treatment
Dr. Katherine Li, a specialist in dry eye and ocular surface diseases, emphasizes that diagnosing MGD isn’t always straightforward. “Many patients come in thinking they just have general dry eye syndrome, but once we examine the lids, it’s clear that their meibomian glands are clogged or atrophied.” Dr. Li explains that examining the structure of the glands via specialized imaging or simply pressing gently on the eyelids can reveal a lot about the health of these critical oil producers.
Treatment options for MGD often begin with self-care measures. Warm compresses, which are used to loosen up blocked glands, and eyelid massages can help express oil. Beyond this, doctors often prescribe oral antibiotics or topical medications that help modify the oil composition and reduce inflammation. More advanced in-office procedures, like LipiFlow, use thermal pulsation to gently heat and massage the glands, offering a mechanical way to clear blockages.
MGD in Action: Real Situations and What Patients Should Know
Consider a common situation: A middle-aged office worker with persistent eye discomfort. Spending long hours in front of a computer screen, her meibomian glands became dysfunctional, reducing oil production and causing a disrupted tear film. After a month of increasingly dry eyes, she visited an eye specialist, who prescribed eyelid hygiene and omega-3 supplements to improve the quality of the oil produced by the glands. This scenario isn’t a one-off—it’s something ophthalmologists report seeing daily in their practices.
Another typical case is that of long-term contact lens wearers. Contact lenses can interfere with the blink mechanism, reducing the ability of the meibomian glands to secrete oil effectively. In these patients, switching to daily disposable lenses and incorporating regular breaks from contact lenses can significantly alleviate symptoms. Dr. Marcus Brown, an optometrist, notes that patients are often surprised at the difference lid hygiene and occasional breaks make in comfort levels.
The Long-Term Effects of Untreated MGD
MGD isn’t just about a bit of discomfort; left untreated, it can lead to serious long-term consequences. Chronic Inflammation is a huge concern. When the meibomian glands stay blocked, they can become inflamed, causing blepharitis (inflammation of the eyelid margin) and even leading to gland atrophy. If enough glands atrophy, it may be impossible to restore their function, leading to permanent dry eye.
Studies have shown that individuals with advanced MGD often suffer from a significant decrease in quality of life due to persistent discomfort, difficulty reading, and a reduced ability to tolerate contact lenses. The psychological impact is also notable, with many patients reporting increased anxiety and stress linked to their ongoing struggle with eye irritation.
Our Editorial Advice: How to Take Control of MGD
Our recommendation? Be proactive. MGD often develops slowly, and early intervention can prevent worsening symptoms. Follow these simple guidelines to take control of your meibomian gland health:
- Blink More Consciously: Whether you’re working or relaxing, take blink breaks every 20 minutes to ensure your glands get activated.
- Warm Compress Routine: Establish a habit of applying warm compresses for 5-10 minutes daily. It’s one of the simplest and most effective ways to keep the oil flowing.
- Dietary Considerations: Consider taking omega-3 supplements. These healthy fats can significantly improve the quality of oil produced by your glands.
- Reduce Screen Time: Easier said than done, but reducing extended periods in front of screens—or at least setting up reminders to blink or take breaks—can make a major difference.
MGD may be common, but with the right knowledge and proactive care, it doesn’t have to take control of your life. Consult with an eye specialist if you’re experiencing symptoms, and start treating your eyes with the attention they deserve.