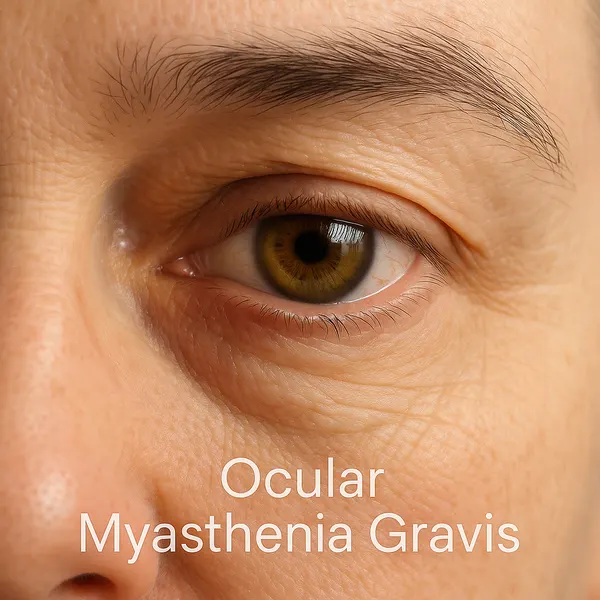
Think of ocular myasthenia gravis (OMG) as a glitch in your body’s electrical wiring — except the lights that flicker are your eyelids and eye muscles. It’s a localized version of a broader autoimmune condition, myasthenia gravis, but this one zeroes in on the tiny muscles that help you blink, look around, and keep your eyes aligned. The result? Symptoms like drooping eyelids (ptosis) or double vision (diplopia) that come and go, often playing hide-and-seek with doctors.
Initial Ophthalmologic Symptoms
This chart highlights the initial ophthalmologic symptoms in patients, focusing on ptosis and diplopia. A majority reported diplopia only (50%), followed by a combination of both symptoms (29%), while ptosis alone was the least frequent (21%).
Now, here’s the deal — while OMG may sound a little scary (and yes, untreated it can creep into other muscle groups), the majority of patients respond well to treatment and lead very normal, very human lives. The trick is not ignoring the signs. Because if your vision suddenly feels like a vintage 3D movie without the glasses, it might be time to speak up. Early recognition is key — and that’s actually great news.
Who Gets Ocular Myasthenia Gravis?
OMG can affect individuals of any age but is most commonly seen in younger women (ages 20–40) and older men (ages 60+). According to the Myasthenia Gravis Foundation of America, up to 50% of patients with OMG may eventually develop generalized myasthenia gravis. A population-based study in the U.S. confirmed an incidence of 1.13 per 100,000 persons annually for OMG (PubMed).
What Triggers This Autoimmune Attack?
Imagine your immune system as your body’s personal security team. Most of the time, it does a great job fending off real threats — viruses, bacteria, you name it. But in ocular myasthenia gravis, it gets confused and starts attacking your own eye muscles by mistake. It’s as if your body thinks the doorknob is a burglar — totally harmless, but now under attack.
Specifically, your immune system creates antibodies that block or damage the communication between your nerves and the muscles that control your eyes. This scrambled signal is why your eyelids might droop or your vision doubles up (Neurology Journal). The key troublemakers? Proteins called acetylcholine receptors, and sometimes MuSK — think of them as the locks on a door that the nerve “keys” are supposed to fit into. When antibodies jam those locks, the message can’t get through.
Why does this happen? Sometimes it’s inherited, sometimes the thymus gland (which helps regulate immunity) acts up, and sometimes it’s triggered by medications or even infections. The Mayo Clinic has shown that thymic abnormalities are especially common in younger patients with OMG (Mayo Clinic Proceedings). It’s not your fault — and it’s not something you can catch from someone else. The encouraging part? Doctors understand a lot more about these triggers now than they did even a decade ago, and that means more ways to treat and manage it.
How Is Ocular Myasthenia Gravis Diagnosed?
Diagnosis of OMG can be tricky — it’s often a case of putting together clinical clues with precision.
Diagnostic Methods:
- Ice Pack Test: Applying an ice pack to the drooping eyelid for 2–5 minutes may temporarily improve ptosis — a quick and simple in-office clue. Accuracy: 7/10; Cost: $0–$10. Supported by data from the Journal of Neuro-Ophthalmology showing a sensitivity between 76%–100% (JNO).
- Antibody Testing: Blood tests to detect anti-AChR or anti-MuSK antibodies. Accuracy: 8/10; Cost: $150–$300. Often the first confirmatory lab tool used.
- Electromyography (EMG): Specifically, single-fiber EMG assesses the electrical activity between muscle fibers. Accuracy: 9/10; Cost: $1,000–$1,500. Recognized by the American Association of Neuromuscular & Electrodiagnostic Medicine as the gold standard (AANEM).
- CT or MRI of the Chest: To rule out thymoma. Accuracy: 9/10; Cost: $500–$1,200. Thymic imaging is critical in assessing systemic risk.
Practical Table: OMG Diagnostic Tools Comparison
| Test | What It Does | Accuracy (1–10) | Cost (USD) | What to Expect During the Test |
|---|---|---|---|---|
| Ice Pack Test | Detects improvement in drooping eyelid (ptosis) by cooling muscle activity | 7 | $0–$10 | Ice pack is placed on the eyelid for 2–5 minutes. Feels cold but painless. Results are immediate. |
| Antibody Testing | Checks for presence of antibodies against AChR or MuSK | 8 | $150–$300 | Simple blood draw. Minimal discomfort. Results typically ready in a few days. |
| Single-fiber EMG | Measures the electrical communication between nerve and muscle fibers | 9 | $1,000–$1,500 | Involves inserting fine needle electrodes into muscles. Mild discomfort. Results same day or next. |
| Chest CT/MRI | Images the chest to check for a thymoma (tumor in thymus gland) | 9 | $500–$1,200 | Non-invasive scan. CT involves X-rays; MRI uses magnets. Usually takes 30–60 min. Results in 1–2 days. |
A recent case from Phoenix, AZ involved a 35-year-old female presenting with intermittent double vision. After three months of misdiagnosis, single-fiber EMG confirmed OMG, and further testing ruled out generalized involvement.
What Are the Latest Treatment Options?
Treatment aims to improve muscle strength and prevent progression to generalized myasthenia gravis. While classic options like corticosteroids remain staples, newer innovations are changing the game.
Pyridostigmine (Mestinon)
This cholinesterase inhibitor works by increasing the amount of acetylcholine at the neuromuscular junction, improving muscle contraction. It’s typically taken orally, two to four times a day, often with food to reduce gastrointestinal side effects.
Patients usually start feeling relief within 30–60 minutes of ingestion, but the effect wears off in about 3–4 hours, requiring repeat doses. Side effects may include cramping, diarrhea, and increased salivation. While not curative, it can dramatically improve daily function when used consistently (Drugs.com).
Prednisone
A corticosteroid used when symptoms are moderate to severe or don’t respond well to pyridostigmine. It’s often started at a low dose and gradually increased. The treatment might begin every other day to reduce long-term risks such as weight gain, high blood pressure, and glucose intolerance.
Improvement may take several days to weeks. Patients must be monitored regularly for side effects and dosage adjustments. It’s often used in tandem with other immunosuppressants for long-term control (NIH MedlinePlus).
Rituximab (Rituxan)
This monoclonal antibody targets CD20-positive B cells, which play a role in antibody production. It is especially beneficial in patients with MuSK antibody-positive OMG who don’t respond to conventional therapies.
Administered via IV infusion, sessions are typically spaced weeks apart. Patients might feel fatigue or mild flu-like symptoms afterward. It requires clinic visits and premedication to reduce infusion-related reactions. Though costly, it has shown high efficacy in refractory cases (Annals of Neurology).
Efgartigimod (Vyvgart) and Ravulizumab (Ultomiris)
These cutting-edge biologics offer targeted immune suppression. Vyvgart reduces IgG antibodies, including the pathogenic ones in MG, while Ultomiris blocks complement activation, a downstream immune response.
Vyvgart is administered via IV once a week for four weeks, and then repeated based on symptom recurrence. Ultomiris is infused every eight weeks after an initial loading phase. Both treatments are generally well-tolerated, though patients should be screened for infections beforehand.
These therapies are reshaping treatment for generalized MG and are under study for OMG, promising precision care with fewer systemic effects (FDA).
How Is Quality of Life Affected?
Fluctuating symptoms can make OMG feel like a guessing game. Patients may wake up symptom-free but experience ptosis by afternoon. This variability can affect work, driving, and social interactions.
A 2023 study from Johns Hopkins found that patients with OMG reported significantly reduced visual-related quality of life scores compared to those with other ocular disorders (Johns Hopkins Medicine).
OMG Cases Progressing to Generalized MG
The chart presents data on the progression of ocular myasthenia gravis (OMG). It shows that 60% of patients generalize to full MG within two years, while 40% retain ocular-only symptoms.
Real Talk: Living with Ocular Myasthenia Gravis
Patients often describe it as having a “lazy eye” that’s unpredictable. One 62-year-old man from Austin, TX shared how he had to give up his favorite pastime — golf — due to unreliable vision.
Support groups and patient education are crucial. Online communities like Myasthenia Gravis News Forums provide shared experiences and practical tips.
Editorial Advice
Reyus Mammadli, medical consultant, recommends early EMG testing if symptoms persist beyond two weeks — “Don’t wait for diplopia to become a daily guest. Early diagnosis is your best defense.”
For newly diagnosed patients, maintaining a symptom diary and communicating clearly with your neurologist can make a world of difference. Adjustable prism glasses may help manage diplopia.
So, stay alert for changes beyond the eyes — even small shifts may signal broader involvement. With the right care, most patients with ocular myasthenia gravis can lead full and active lives.
MG Mortality Rate Today
This chart displays current in-hospital mortality rates for myasthenia gravis. While the overall mortality remains low at 2.2%, patients experiencing a myasthenic crisis face a significantly higher risk at 4.5%.



