Intraocular pressure (IOP) is the fluid pressure inside the eye. Tonometry is the approach eye care specialists use to determine this. IOP is an important aspect in the examination of patients at risk from glaucoma. Most tonometers are adjusted to measure pressure in millimeters of mercury (mmHg).
What Is Intraocular Pressure
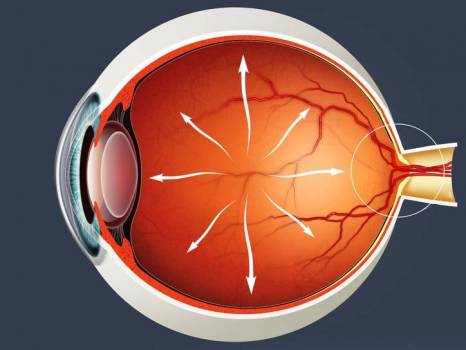
Intraocular pressure is primarily determined by the coupling of the production of aqueous humour and the drainage of liquid humour generally through the trabecular meshwork located in the anterior chamber angle. The reason for this is because the vitreous humour in the posterior section has a fairly set volume and hence does not impact intraocular pressure regulation.
An important quantitative relationship is shown below:
IOP = F/C + PV
Where F = liquid fluid formation rate, C = outflow rate, PV = episcleral venous pressure. The above aspects are those that own IOP.
How Is Intraocular Pressure Measured?
Intraocular pressure is measured with a tonometer as part of a thorough eye assessment.
Determined values of intraocular pressure are influenced by corneal density and rigidity. As an outcome, some kinds of refractive surgery (such as photorefractive keratectomy) can cause standard intraocular pressure measurements to appear normal when in fact the pressure might be unusually high. A newer transpalpebral and transsleral tonometry technique is not influenced by corneal biomechanics and does not need to be changed or corneal abnormalities as measurement is done over upper eyelid and sclera.
Normal Intraocular Pressure in Human
Existing consensus among ophthalmologists and eye doctors define normal intraocular pressure as that in between 10 mmHg and 20 mmHg. The average worth of intraocular pressure is 15.5 mmHg with changes of about 2.75 mmHg.
Ocular hypertension (OHT) is specified by intraocular pressure being greater than normal, in the absence of optic nerve damage or visual field loss.
Ocular hypotension, Hypotony, or ocular hypotony, is typically defined as intraocular pressure equivalent to or less than 5 mmHg. Such low intraocular pressure might suggest fluid leak and deflation of the eyeball.
Affecting Factors
Daily variation
Intraocular pressure differs throughout the night and day. The diurnal variation for normal eyes is between 3 and 6 mmHg and the variation may increase in glaucomatous eyes. During the night, intraocular pressure might not reduce in spite of the slower production of liquid humour. In the basic population, IOP ranges in between 10 and 21 mm Hg with a mean of about 15 or 16 mm Hg (plus or minus 3.5 mm Hg during a 24-hour cycle).
Physical fitness and workout
There is some undetermined research that indicates that workout might perhaps affect IOP (some favorably and some negatively). Nevertheless, some other types of workout might raise IOP.
Musical instruments
Playing some musical wind instruments has actually been connected to boosts in intraocular pressure. One 2011 study focused on brass and woodwind instruments observed “temporary and sometimes dramatic elevations and variations in IOP”. Another research study found that the magnitude of boost in intraocular pressure associates with the intraoral resistance associated with the instrument, and connected periodic elevation of intraocular pressure from playing high-resistance wind instruments to incidence of visual field loss. The range of intraoral pressure involved in various classes of ethnic wind instruments, such as Native American flutes, has been shown to be generally lower than Western classical wind instruments.
Drugs
Intraocular pressure likewise varies with a number of other elements such as heart rate, respiration, fluid consumption, systemic medication and topical drugs. Alcohol and cannabis consumption results in a transient decrease in intraocular pressure and caffeine might increase intraocular pressure.
Taken orally, glycerol (often mixed with fruit juice to reduce its sweet taste) can cause a rapid, temporary reduction in intraocular pressure. This can be an useful preliminary first aid of significantly elevated pressure.
The depolarising muscle relaxant succinylcholine, which is used in anaesthesia, transiently increases IOP by around 10mmHg for a couple of minutes. This is significant for example if the patient requires anaesthesia for an injury and has sustained an eye (world) perforation. The system is unclear however it is thought to involve contraction of tonic myofibrils and short-term dilation of choroidal blood vessels.
Complications
Ocular hypertension is the most crucial risk element for glaucoma.
Intraocular pressure has been measured as a secondary result in a systematic review comparing the result of neuroprotective agents in slowing the progression of open angle glaucoma.
Differences in pressure in between the two eyes are often clinically substantial, and potentially connected with specific types of glaucoma, in addition to iritis or retinal detachment.
Intraocular pressure might become raised due to anatomical issues, swelling of the eye, hereditary factors, or as a side-effect from medication. Intraocular pressure laws follow fundamentally from physics. Any kinds of intraocular surgery should be done by considering the intraocular pressure fluctuation. All of a sudden increase of intraocular pressure leads to intraocular micro barotrauma and causing anemia impact and mechanical stress to retinal nerve fiber layer. Rapid intraocular pressure drop leads to intraocular decompression that produces micro bubble that potentially triggering numerous micro emboli and resulting in hypoxia, anemia and retinal micro structure damage.