Optic disc drusen (ODD) or optic nerve head drusen (ONHD) are globules of mucoproteins and mucopolysaccharides that progressively calcify in the optic disc. They are believed to be the remnants of the axonal transportation system of degenerated retinal ganglion cells. ODD have likewise been described as congenitally elevated or anomalous discs, pseudopapilledema, pseudoneuritis, buried disc drusen, and disc hyaline bodies. They might be associated with vision loss of differing degree occasionally resulting in blindness.
Optic Disc Drusen Causes
The optic nerve is a cable tube connection that transmits images from the retina to the brain. It includes over one million retinal ganglion cell axons. The optic nerve head, or optic disc is the anterior end of the nerve that remains in the eye and for this reason shows up with an ophthalmoscope. It lies nasally and somewhat inferior to the macula of the eye. There is a blind spot at the optic disc since there are no rods or cones below it to discover light. The main retinal artery and vein can be seen in the middle of the disc as it exits the scleral canal with the optic nerve to provide the retina. The vessels send branches out in all directions to supply the retina.
How Often Does ODD Occur?
Optic disc drusen are found scientifically in about 1% of the population but this increases to 3.4% in people with a family history of ODD. About two thirds to 3 quarters of clinical cases are bilateral. A necropsy research study of 737 cases revealed a 2.4% incidence with 2 from 15 (13%) bilateral, maybe suggesting the perilous nature of many cases. An autosomal dominant inheritance pattern with incomplete penetrance and associated acquired dysplasia of the optic disc and its blood supply is suspected.
Males and females are affected at equivalent rates. Caucasians are the most vulnerable ethnic group. Particular conditions have actually been connected with disc drusen such as retinitis pigmentosa, angioid streaks, Usher syndrome, Noonan syndrome and Alagille syndrome. Optic disc drusen are not connected to Bruch membrane drusen of the retina which have actually been connected with age-related macular degeneration.
Age-Related Optic Disc Drusen
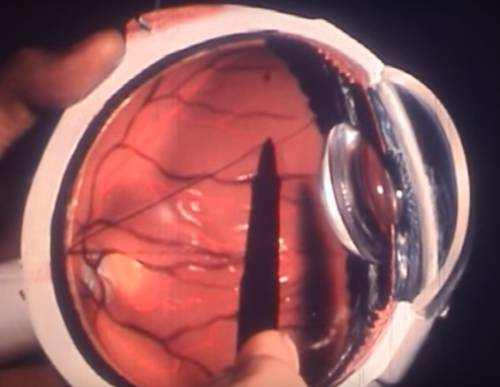
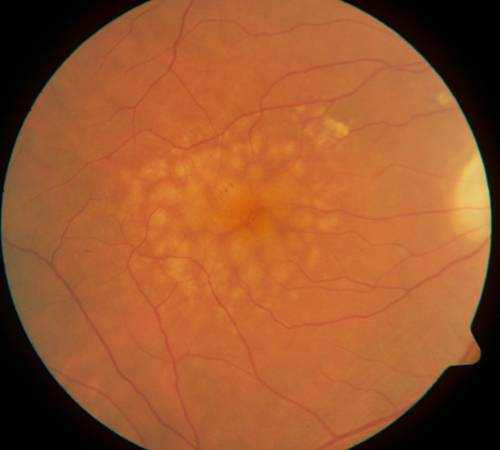
In children, optic disc drusen are usually buried and undectectable by fundoscopy except for a mild or moderate elevation of the optic disc. With age, the overlying axons end up being atrophied and the drusen become exposed and more visible. They may emerge with an ophthalmoscope and some visual field loss at the end of adolescence. ODD can compress and eventually jeopardize the vasculature and retinal nerve fibers. Hardly ever, choroidal neovascularization might establish as the juxtapapillary nerve fibers are interrupted, with subsequent subretinal hemorrhage and retinal scarring. Even more rarely, vitreous hemorrhage might develop.
Optic Disc Drusen Prognosis and Diagnosis
Optic nerve damage is progressive and perilous. Ultimately 75% of patients will develop some peripheral field problems. These can include nasal step problems, enlarged blind spots, arcuate scotomas, sectoral field loss and altitudinal flaws. Medical symptoms associate to presence of the drusen. Central vision loss is an unusual issue of bleeding from peripapillar choroidal neovascular membranes. Anterior ischemic optic neuropathy (AION) is a prospective issue.
In a lot of patients, optic disc drusen are an incidental finding. It is very important to differentiate them from other conditions that present with optic disc elevation, particularly papilledema, which might indicate raised intracranial pressure or tumors. True papilledema might present with exudates or cotton-wool spots, unlike ODD. The optic disc margins are characteristically irregular in ODD but not blurred as there is no swelling of the retinal nerve fibers. Spontaneous venous pulsations exist in about 80 percent of patients with ODD, but absent in cases of true disc edema.
Other causes of disc elevation clinicians must omit might be: hyaloid traction, epipapillary glial tissue, myelinated nerve fibres, scleral infiltration, vitreopapillary traction and high hyperopia. Disorders connected with disc elevation include: Alagille syndrome, Down syndrome, Kenny-Caffey syndrome, Leber Hereditary Optic Neuropathy and linear nevus sebaceous syndrome.
How to Deal with Optic Disc Drusen?
Patients with optic disc drusen should be kept an eye on periodically for ophthalmoscopy, Snellen skill, contrast sensitivity, color vision, intraocular pressure and limit visual fields. For those with visual field defects optical coherence tomography has been suggested for follow up of nerve fiber layer thickness. Associated conditions such as angioid streaks and retinitis pigmentosa need to be screened for. Both the severity of optic disc drusen and the degree of intraocular pressure elevation have been related to visual field loss.
There is no widely accepted treatment for ODD, although some clinicians will recommend eye drops designed to reduce the intra-ocular pressure and in theory alleviate mechanical stress on fibers of the optic disc. Hardly ever choroidal neovascular membranes may develop surrounding to the optic disc threatening bleeding and retinal scarring. Laser treatment or photodynamic therapy or other progressing therapies may prevent this problem.