Phlyctenulosis may sound like the name of an obscure ancient city, but in reality, it’s an immune response that can affect your eyes — and it’s more common than you’d think. This condition is characterized by the appearance of small, raised, red or yellowish-white nodules (phlyctenules) on the conjunctiva or cornea. These nodules typically form near the limbus, where the white part of the eye meets the colored part.
Immune Mechanism of Phlyctenulosis (Timeline in Days)
So why does this happen? It’s basically your body’s immune system overreacting to certain antigens — often bacterial, such as Staphylococcus aureus or Mycobacterium tuberculosis. It’s the eye’s way of saying, “Hey, I don’t like what you’re doing here!”
Although phlyctenulosis is usually self-limiting and non-contagious, it can be quite uncomfortable and, if left untreated, may lead to complications like corneal scarring. That’s why knowing the signs and seeking early treatment matters.
Who’s Most Likely to Develop It?

While phlyctenulosis can technically occur at any age, it’s most frequently seen in children and young adults. Girls under 16 are particularly more susceptible, especially those with chronic staph blepharitis (inflammation of the eyelid margins). In regions where tuberculosis is still prevalent, TB-related phlyctenulosis is also more common.
Age & Gender Profile of Pediatric Phlyctenulosis
A real-life example: A 12-year-old girl from rural New Mexico was brought to her ophthalmologist for recurrent eye redness and irritation. She was initially misdiagnosed with conjunctivitis. Upon closer examination and detailed history, doctors discovered she had chronic staphylococcal blepharitis and was developing phlyctenules on her cornea — a classic setup for phlyctenulosis.
Environmental and personal hygiene factors also play a significant role. Poor eyelid hygiene, exposure to irritants, and even vitamin A deficiency have been associated with higher risk.
What Symptoms Should You Look Out For?
Phlyctenulosis may be mistaken for more common eye conditions like conjunctivitis or dry eye, but it has its own unique symptom profile. Understanding the nuances of each symptom can help in early identification.
- Redness and tearing in the affected eye: This is the most common and noticeable symptom. The redness is usually localized around the limbus and may be accompanied by watery discharge. This symptom is often present throughout the day and tends to persist until the phlyctenule resolves.
- Light sensitivity (photophobia): This symptom is particularly telling when the cornea is involved. It’s often described as a sharp sensitivity to indoor or outdoor light and may worsen in the early morning. Its presence strongly suggests corneal phlyctenulosis and should raise concern for deeper inflammation.
- Burning or stinging sensation: These sensations are usually mild to moderate and can be mistaken for allergies. In phlyctenulosis, they are more consistent and tend to occur regardless of environmental triggers, often peaking in the evening.
- Foreign body sensation: Patients often feel as if something is stuck in the eye — a scratchy, gritty feeling that doesn’t go away with blinking or eye drops. This symptom usually appears early in the episode and is highly characteristic of phlyctenules located on the cornea.
- Mild pain or discomfort: Pain is typically not severe but may increase with blinking or eye movement. This is a secondary symptom and less common than irritation or photophobia, but if pain becomes sharp or constant, it may indicate ulceration.
How to Weigh These Symptoms
| Symptom | Frequency | Severity Indicator | Diagnostic Weight |
|---|---|---|---|
| Redness & tearing | High | Persistent, daily | Primary symptom |
| Photophobia | Moderate–High | More pronounced in mornings | Strong indicator of corneal involvement |
| Burning/stinging | Moderate | Mild–worsens in evening | Secondary symptom |
| Foreign body sensation | High | Occurs early, persistent | Highly characteristic |
| Pain | Low–Moderate | Increases if ulcer forms | Supplementary, requires monitoring |
If two or more of the primary symptoms — especially redness, photophobia, and foreign body sensation — occur together and last more than 48 hours without improvement, it’s a strong cue to visit an ophthalmologist.
Many patients mistake these signs for eye strain or seasonal allergies, delaying proper care. Reyus Mammadli, medical consultant, emphasizes: “With phlyctenulosis, it’s all about the pattern. If symptoms are consistent, one-sided, and don’t respond to lubricants — it’s time to get your eyes examined.”
How Is Phlyctenulosis Diagnosed?
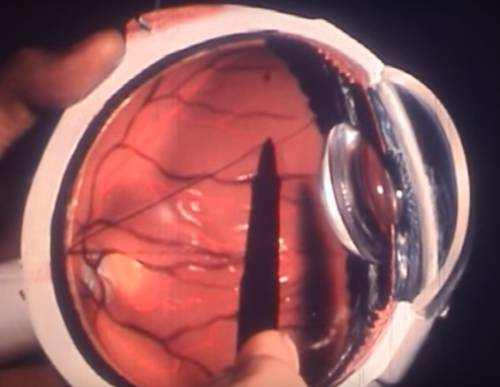
Diagnosing phlyctenulosis involves a combination of clinical evaluation and targeted history-taking. An ophthalmologist typically performs a slit-lamp examination to visualize the lesion in detail.
Common Diagnostic Methods
| Method | Description | Accuracy (1–10) | Avg. Cost (USD) |
|---|---|---|---|
| Slit-lamp exam | High-resolution exam of anterior segment | 9/10 | $80–$150 |
| Conjunctival scraping | For microbiological analysis | 7/10 | $150–$300 |
| PPD (tuberculin skin test) | To rule out TB cause | 8/10 | $20–$60 |
| Chest X-ray | If TB is suspected | 9/10 | $100–$250 |
| Lid margin culture | Identifies staph or other bacteria | 7/10 | $120–$180 |
Some newer clinics now use in vivo confocal microscopy (IVCM), a non-invasive technique offering near-histological detail of ocular tissues. While it’s still expensive (around $400), it helps detect corneal involvement earlier. ⧉
What to Expect from Each Diagnostic Method
- Slit-lamp exam: This is a routine, painless exam where the patient rests their chin on a support while the doctor uses a special microscope and light to closely inspect the front of the eye. It takes about 5–10 minutes and does not require dilation.
- Conjunctival scraping: A small sample is gently taken from the surface of the eye using a sterile spatula. It may cause mild discomfort, similar to a scratchy sensation, and results are usually available within 48–72 hours if sent to a lab.
- PPD (tuberculin skin test): This test involves a tiny injection under the skin of your forearm. It’s quick, feels like a small pinch, and you’ll need to return after 48–72 hours for the result, which is a simple visual inspection.
- Chest X-ray: A standard imaging procedure done while standing against a plate, usually completed in under 15 minutes. It’s non-invasive, and results can be ready the same day or within 1–2 days.
- Lid margin culture: A swab is gently rubbed along the edge of your eyelid to collect bacteria. It causes little to no pain, and results are generally returned in 48–72 hours.
The Latest in Treatment and Management
Here’s the good news: most cases respond well to topical therapy. Treatment aims to eliminate the underlying antigen and calm the immune response.
Topical Corticosteroids
Topical corticosteroids like prednisolone acetate 1% or loteprednol etabonate are commonly prescribed to reduce inflammation. Think of them as the eye’s version of a fire extinguisher — they don’t solve the root problem but are highly effective at calming the flare. Treatment typically lasts 7–10 days, with drops applied 2–4 times daily. Patients usually begin to notice improvement within 48 hours. However, these drops only address inflammation — not the cause — so they’re often used in conjunction with other treatments.
Antibiotic Drops or Ointments
These target the bacterial component of the condition, especially Staphylococcus aureus. Medications like tobramycin or erythromycin are applied to the eyes or lids. Think of antibiotics here as the bouncers that remove the troublemakers causing the immune reaction. They’re generally used for 1–2 weeks and can be very effective in breaking the cycle of inflammation when the condition is linked to blepharitis or lid infections.
Lid Hygiene
Daily eyelid cleaning — with diluted baby shampoo or over-the-counter lid scrubs — is essential. It’s a long-term strategy, like brushing your teeth daily to avoid cavities. Lid hygiene doesn’t just prevent flare-ups; it treats the root problem by removing bacteria and debris that contribute to chronic eyelid inflammation. Most patients need to continue this indefinitely, especially if prone to recurrent phlyctenulosis.
Oral Antibiotics
In recurrent or more stubborn cases, oral antibiotics like doxycycline or azithromycin are prescribed. Doxycycline, for example, has both antibacterial and anti-inflammatory properties. This approach is often used in adults and older teens. Treatment usually lasts from 2 to 6 weeks. It’s a more systemic strategy — like calling in reinforcements to help patrol the entire body — and is especially helpful when topical treatments alone aren’t enough.
For TB-related phlyctenulosis, systemic anti-tubercular therapy (ATT) is crucial. In the U.S., this typically includes isoniazid, rifampin, pyrazinamide, and ethambutol under CDC guidelines ⧉.
Reyus Mammadli, medical consultant, notes: “In modern practice, the key is not just symptom relief but identifying the antigenic trigger. Otherwise, you’re just playing whack-a-mole with the immune response.”
Can Phlyctenulosis Recur — and How Do You Stop It?
Yes, phlyctenulosis can definitely come back — and often does if the root cause isn’t properly addressed. This condition isn’t a one-time event like a cold; it’s more like a recurring allergic reaction. Think of it like weeds in your garden — if you only trim the top but don’t pull out the roots, they’ll be back before you know it.
The most common causes of recurrence include untreated blepharitis, inconsistent lid hygiene, and systemic infections like tuberculosis that haven’t been fully managed. In many cases, the recurrence doesn’t happen randomly but follows a pattern — often reappearing during periods of stress, illness, or lapses in daily eyelid care.
Patients who skip their hygiene routines or stop treatment too early are far more likely to experience repeated episodes. Maintenance strategies, such as continued lid scrubs, periodic antibiotic use, or anti-inflammatory drops, help reduce recurrence dramatically — but only if applied consistently.
Reyus Mammadli, medical consultant, emphasizes: “Phlyctenulosis recurrence is less about bad luck and more about long-term discipline. Think of daily lid hygiene as dental floss for your eyelids — not exciting, but essential.”
Maintenance with occasional low-dose steroid drops or oral antibiotics may be necessary for chronic sufferers.
Possible Complications of Phlyctenulosis in Children
When to See a Doctor Immediately
Most cases of phlyctenulosis aren’t emergencies, but some symptoms act like flashing red lights on your dashboard — they mean something serious could be going on underneath the surface. Here’s what to watch for, and what each warning sign may indicate:
- Sudden, severe eye pain: This isn’t the usual irritation or gritty feeling. If the pain comes on abruptly and feels sharp or deep, it could be a sign of corneal ulceration or inflammation extending beyond the surface. In phlyctenulosis, pain usually stays mild — so anything intense should raise alarm.
- Rapid vision changes: Blurred or reduced vision in one eye over a short period (hours to a day) may signal involvement of the visual axis or corneal opacity. While mild phlyctenulosis doesn’t typically affect vision, sudden change suggests possible complications or deeper corneal involvement.
- Ulceration or discharge: A visible lesion that starts to break down (ulcerate), or thick yellow-white discharge, could indicate secondary bacterial infection or corneal damage. This combination raises the risk of permanent scarring.
- Symptoms not improving with treatment in 5–7 days: If you’re already using prescribed medications and don’t see clear improvement within a week, this could mean the underlying cause hasn’t been properly identified — such as TB-related inflammation or antibiotic resistance.
When These Symptoms Combine
A single red flag is enough to warrant a visit, but combinations should not be ignored. For example:
- Severe pain + vision changes: May indicate progressing ulcer or keratitis.
- Ulceration + discharge: High risk of bacterial superinfection.
- Photophobia + no response to steroids: Possibly deeper corneal inflammation or misdiagnosis.
In any of these scenarios, delay in care can lead to irreversible damage — including permanent vision loss. As Reyus Mammadli, medical consultant, puts it: “Don’t play the waiting game with your eyes. If things get worse fast, get help faster.”
Never attempt to self-treat with over-the-counter redness drops or old medications. These may mask symptoms while the condition quietly worsens underneath.
Editorial Advice
Reyus Mammadli, medical consultant, recommends a “two-pronged approach” — treat the flare, and eliminate the trigger. “Think of it like allergy management. You wouldn’t just use antihistamines without addressing the dust mites, right?”
For patients, that means staying consistent with eyelid hygiene, attending follow-ups, and ensuring any systemic illness (like TB) is thoroughly managed. Kids, especially, need help from caregivers to keep up with preventive measures.
Other tips include:
- Use warm compresses daily during flare-ups
- Never skip prescribed medications
- Avoid rubbing your eyes, even if they itch
- Watch for early signs of recurrence and report them
As long as the immune system keeps doing its thing, phlyctenulosis may show up uninvited. But with smart strategies and medical support, you can definitely keep it from overstaying its welcome.