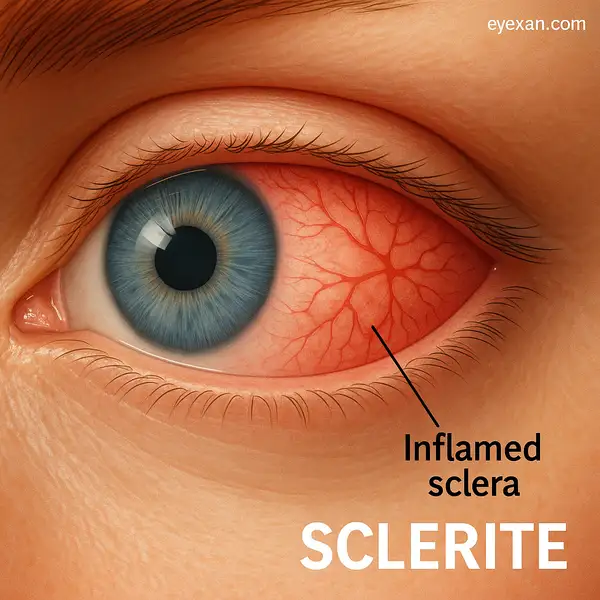
Sclerite might not be a household word, but if you’ve ever felt a deep, throbbing pain in your eye that just won’t quit, this condition may be the culprit. Affecting the white outer layer of the eye (the sclera), sclerite is more than just a case of redness—it’s a potentially vision-threatening disease. While it’s not as common as conjunctivitis or dry eye syndrome, it demands attention because of its strong ties to systemic diseases and its tendency to cause long-term damage if untreated.
What Is Sclerite and Why Does It Matter?
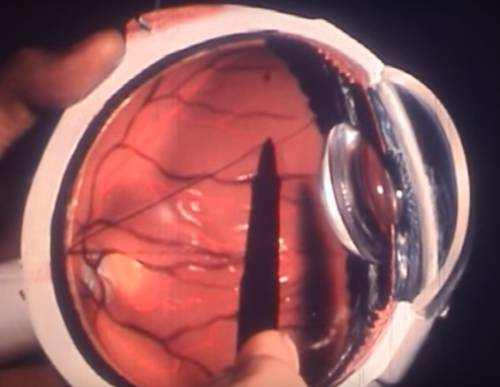
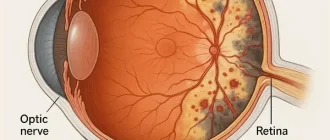
Sclerite is an inflammatory disorder of the sclera, the protective white covering that gives the eye its structure. Unlike episcleritis (a much milder inflammation that usually resolves on its own), sclerite is severe, painful, and often connected to autoimmune diseases. Patients frequently describe the pain as radiating from the eye into the jaw or temple, sometimes bad enough to wake them up at night. That’s not your typical eye irritation—it’s a red flag.
The condition can affect either one or both eyes, with a higher prevalence in women between the ages of 30 and 60. Left unchecked, the inflammation can thin the sclera, leading to dangerous complications such as perforation or even permanent vision loss.
Common Causes and Risk Factors of Sclerite
The origins of sclerite are usually systemic, meaning they often come from something larger than the eye itself. Around half of cases are linked to autoimmune diseases, with rheumatoid arthritis being the top offender. Other culprits include lupus, granulomatosis with polyangiitis, and inflammatory bowel disease.
Infectious causes are less common but still relevant—herpes zoster, tuberculosis, and syphilis can all trigger sclerite. Trauma, surgery, and certain medications can also set off the condition. Statistically, women in their middle years have a slightly higher risk, and about 36% of cases are bilateral.
Typical Symptoms: How to Spot It Early
Patients with sclerite often know something is wrong right away—it’s not the kind of discomfort you ignore. The primary symptom is a deep, boring eye pain that worsens with movement or at night. Unlike conjunctivitis, the redness in sclerite is more localized and violaceous (purple-red). Additional signs include photophobia (light sensitivity), decreased vision, and sometimes excessive tearing.
Take the example of a 45-year-old woman from Dallas, TX, who was initially treated for “chronic conjunctivitis.” After weeks of worsening pain and blurred vision, a referral to a specialist confirmed diffuse anterior sclerite. Her case highlights the importance of early, accurate diagnosis.
How Is Sclerite Diagnosed?
Diagnosing sclerite requires more than a quick glance. Ophthalmologists rely on a combination of patient experience, careful eye examination, and modern imaging tools:
- Slit-lamp exam: The doctor uses a special microscope with a bright beam of light to zoom in on the eye’s surface. Patients typically feel no pain, just the slight discomfort of sitting still while the light shines directly in the eye. Results are immediate, allowing the ophthalmologist to see whether the redness comes from superficial vessels or deeper layers of the sclera.
- Ultrasound (B-scan): This test uses sound waves to create images of the back of the eye. A small probe, often placed gently on the closed eyelid with gel, sends signals that bounce back to form a picture. Patients may feel cool gel and mild pressure, but it’s quick and noninvasive. Results are available within minutes.
- MRI of the orbit: Much like an MRI for the knee or spine, this imaging technique uses powerful magnets to show detailed structures around the eye. Patients lie inside the MRI scanner for 20–40 minutes. The process is painless but noisy, and results usually take a day or two to be reviewed. MRI is especially good at detecting scleral thickening and surrounding tissue inflammation.
- CT scan: A CT uses X-rays to produce cross-sectional images of the eye socket. Patients lie on a table while the scanner circles around their head—it takes less than 10 minutes. This test is particularly useful to rule out tumors or infections that mimic sclerite. Results are often available the same day.
- Laboratory tests: Blood samples are drawn to check for autoimmune markers such as ANA, RF, or ANCA. The needle prick is the only discomfort, and results typically come back within a few days. These tests don’t confirm sclerite but help uncover underlying systemic conditions.
| Diagnostic Method | Accuracy (1–10) | Avg. Cost (USD/EUR) |
|---|---|---|
| Slit-lamp exam | 7/10 | $150 / 135 € |
| Ultrasound (B-scan) | 8/10 | $200–400 / 180–360 € |
| MRI of orbit | 9/10 | $800–1500 / 730–1370 € |
| CT scan | 7/10 | $500–1000 / 450–900 € |
| Lab tests (autoimmune) | 6/10 | $100–300 / 90–270 € |
According to Reyus Mammadli, medical consultant, using a multimodal diagnostic approach is key: “Don’t rely on a single test; combine imaging and lab results for the most accurate picture.”
Latest Treatment Approaches for Sclerite
Modern management of sclerite is tailored to the underlying cause. Each approach has its own set of medications, expectations for the patient, effectiveness rates, and costs.
Systemic Corticosteroids
What it includes: Corticosteroids such as Prednisone are typically prescribed orally, starting with higher doses and tapering down over weeks to months. In severe cases, intravenous methylprednisolone may be used.
Patient experience: Patients often feel rapid relief of pain within a few days. Side effects may include increased appetite, weight gain, mood swings, or elevated blood sugar.
Effectiveness: Around 70–80% of patients respond well, particularly in the early stages.
Cost: Prednisone tablets are relatively inexpensive, averaging $15–50 (≈14–45 €) per month. IV treatments cost more, typically $200–400 (≈180–360 €) per infusion.
Immunomodulators
What it includes: Drugs like Methotrexate, Azathioprine, and Mycophenolate mofetil are used for patients who either don’t tolerate steroids or need long-term control.
Patient experience: These medications require regular blood tests to monitor liver and kidney function. They are taken orally or by injection. Patients often notice improvement within weeks to months.
Effectiveness: Response rates range from 60–75%. These drugs are especially helpful in cases linked to systemic autoimmune conditions.
Cost: Methotrexate averages $25–80 (≈22–70 €) per month, while newer agents like mycophenolate may cost $300–600 (≈270–550 €) monthly.
Biologic Therapies
What it includes: Biologics such as Adalimumab (Humira) and Infliximab (Remicade) target specific immune pathways. They are administered via injection (Humira) or infusion (Remicade).
Patient experience: Humira is self-injected every 2 weeks, while Remicade requires infusion at a clinic every 6–8 weeks. Patients often feel significant relief within 4–6 weeks.
Effectiveness: Studies show 70–85% success rates, particularly in sclerite linked to rheumatoid arthritis or other autoimmune diseases.
Cost: Biologics are expensive, averaging $4,000–6,000 (≈3,600–5,500 €) per month without financial assistance.
Anti-Infective Therapy
What it includes: If sclerite is caused by infection, treatment involves targeted antibiotics (e.g., ceftriaxone for syphilis) or antivirals (e.g., acyclovir for herpes zoster).
Patient experience: Depending on the infection, patients may need oral or intravenous therapy for several weeks. Relief of symptoms usually follows within 1–2 weeks of starting treatment.
Effectiveness: High when the infection is identified early—often exceeding 90% resolution rates.
Cost: Antibiotics like ceftriaxone may cost $200–500 (≈180–450 €) for a treatment course; antivirals like acyclovir range from $50–150 (≈45–135 €).
Surgical Intervention
What it includes: For severe thinning or risk of rupture, surgeons may perform scleral grafting or patching with donor tissue.
Patient experience: Surgery is usually done under local or general anesthesia. Recovery can involve several weeks of close monitoring and eye drops to prevent infection and rejection.
Effectiveness: Surgical success rates are reported at 75–85%, especially when combined with medical therapy.
Cost: Procedures typically cost $5,000–10,000 (≈4,500–9,000 €), depending on hospital setting and graft material.
Possible Complications If Left Untreated
Ignoring sclerite is like ignoring a smoke alarm—it’s only a matter of time before disaster strikes. Complications include scleral thinning, globe perforation, secondary glaucoma, cataracts, and permanent vision loss. Emotional toll is also significant, as patients often struggle with chronic pain and anxiety about losing their eyesight.
A documented case from Boston, MA, involved a 52-year-old man with untreated posterior sclerite who presented with sudden, severe vision loss. By the time treatment began, irreversible damage had occurred.
Prevention and Lifestyle Adjustments
While not all cases are preventable, patients can reduce their risks by managing systemic conditions effectively. Regular rheumatology and ophthalmology visits are essential for people with known autoimmune diseases. But lifestyle choices matter too—and here, structure is key.
Diet Plan Example for Eye Health
- Morning (7–8 AM): A breakfast with omega-3 rich foods, such as oatmeal topped with ground flaxseeds and a boiled egg. Add a cup of green tea for antioxidants.
- Midday (12–1 PM): Grilled salmon (4 oz / 120 g) with a side of spinach salad. This gives a concentrated dose of omega-3 and lutein.
- Afternoon snack (3–4 PM): A handful of walnuts (1 oz / 28 g) and a small bowl of blueberries for antioxidants.
- Evening (6–7 PM): Baked chicken breast with steamed broccoli and sweet potatoes, balancing protein with carotenoid-rich vegetables.
- Hydration: Aim for 6–8 glasses (1.5–2 liters) of water daily.
This type of routine ensures patients don’t just “take omega-3” but actually spread nutrients throughout the day in effective, balanced doses. Overconsumption can lead to digestive upset or unnecessary calories, so moderation matters.
Duration and Consistency
A diet like this should be maintained for at least 6–8 weeks to notice improvements in overall eye comfort and health. Long-term adherence maximizes benefits and complements medical therapy.
Lifestyle Practices
- Exercise: Light walks (20–30 minutes daily) to support circulation.
- Eye protection: Use sunglasses outdoors to block UV rays.
- Routine check-ups: Patients with autoimmune diseases should plan ophthalmology visits every 6–12 months.
By following a structured plan, patients don’t just “hear” advice like “eat more omega-3”—they know exactly how, when, and how much to consume.
Editorial Advice
Sclerite may sound intimidating, but with modern diagnostics and advanced therapies, outcomes are far better than they used to be. Reyus Mammadli, medical consultant, emphasizes: “Early recognition is the patient’s best ally—don’t dismiss eye pain as something minor.”
The editorial team also recommends practical steps:
- Don’t self-diagnose—see an ophthalmologist if you have persistent eye pain.
- If you live with rheumatoid arthritis or lupus, schedule annual eye checks.
- Keep a record of your systemic health conditions and share them with your eye specialist.
In the end, protecting your vision means paying attention to the subtle (and sometimes not-so-subtle) signs your body is sending. Eye pain is never just “nothing”—treat it with the seriousness it deserves.