Salzmann’s nodular degeneration is unusual, yet potentially sight-threatening condition that may require surgery.
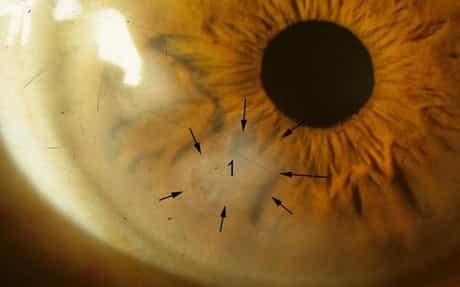
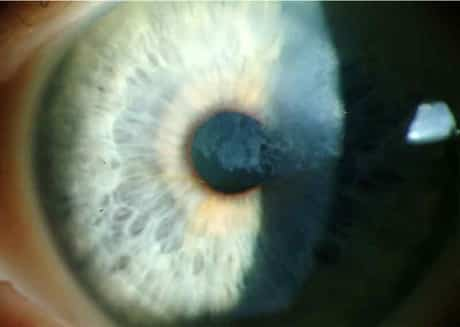
On clinical assessment, Salzmann’s nodular degeneration (SND) appears as superficial, bluish-white, raised sores that are often situated in the peripheral cornea. Patients can experience irritation, such as dryness and foreign body experience, as well as decreased vision in innovative cases.

A medical diagnosis of SND brings a very favorable prognosis, and patients typically wish to know how the condition can be treated. Here, we will examine the current research study about the identification and treatment of SND.
What Is Salzmann’s Nodular Degeneration?
SND is an uncommon, non-inflammatory, gradually progressive, degenerative condition. Women are considerably most likely to experience SND than men. The typical age of presentation is 59 years and the most common symptom connected with SND is a foreign body feeling. Even more, the condition provides bilaterally in 63% of cases.
Confocal microscopy suggests that these sores are elongated basal epithelial cells and activated keratocytes, particularly in the area of the anterior stroma near the blemishes. Occasional sub-basal nerves and tortuous stomal nerve bundles are observed. Spectral domain OCT imaging frequently exposes fibrous intraepithelial blemishes with substantial overlying epithelial thinning, which likely contributes to patients’ symptoms.
Although the patient’s environment may contribute, research suggests that there might be a genetic or familial pattern of development.
Prospective Associations
Recent research study revealed an extremely high association in between patients diagnosed with SND and osteoporosis – recommending that SND might indicate a problem of the client’s mucopolysaccharides. Separate research studies have shown a high correlation to chronic ocular surface area inflammatory conditions, such as keratoconjunctivitis sicca, direct exposure keratopathy, and pterygium. Other scientists have questioned if hyaline degeneration of the cornea may be a precursor to SND. Also, yet other research studies reveal a high connection of SND in patients with epithelial basement membrane dystrophy.
Topical Treatment Options for Salzmann’s Nodules
If patients experience very little irritation, several topical medications can be useful. Artificial tears– especially more concentrated formulas with longer retention times, such as FreshKote (Focus Laboratories) or Blink Gel Tears (AMO) — might help reduce inflammation and discomfort. If patients show symptoms of grittiness, foreign body feeling or even photophobia, topical corticosteroids (e.g., loteprednol 0.5%) and topical NSAIDs (e.g., bromfenac) can be utilized to ease the inflammation and pain.
For long-term management, patients could be treated with cyclosporine A. At this point, topical NSAIDs and corticosteroids would be reserved for more substantial symptom episodes.
Salzmann’s Nodular Degeneration Surgical Treatment
If, however, the blemishes are creating substantial visual disturbances by wrongly modifying the tear movie or triggering irregular astigmatism to the cornea, surgery is recommended.
One of the most successful treatments is either superficial keratectomy (SK), or phototherapeutic keratectomy (PTK) with the application of mitomycin C. Mitomycin C avoids the formation of corneal haze and/or scarring. In one study, these surgical procedures for SND improved mean best-corrected visual acuity from 20/80 to 20/30. Remember, nevertheless, that when these peripheral lesions are gotten rid of, the patient might experience a myopic refraction shift.
When a client provides for surgical removal via SK or PTK, the nodules often different from Bowman’s layer very easily. Other times — especially when vascularization or pannus is presented – the SND lesions can leave a large defect that typically will require excimer laser treatment to remove any irregularity. The reoccurrence rate of SND following PTK is low and approximated to be about 20% within 12 years of surgery. Fortunately, corneal and lamellar transplant is rarely needed for patients with SND.
O.D.s in primary care settings frequently identify SND, so it is essential to comprehend its pathogenesis and associated manifestations. Having the ability to keep track of and educate patients, in addition to suggesting a suitable treatment, is critical.
I have been diagnosed with Salzmann’s nodular degeneration. It is rare. I am searching for a professional in this. When I get a flareup, nasal allergy symptoms come with the feeling of gravel in my eye. If I deal with bad nasal symptoms, eyes get worse because of antihistamines and decongestants. However, there are times I can take these medications with no eye issues. The last flareup also consisted of new symptoms:
1. swelling of the eyes up until practically shut.
2. dangerous level of sensitivity to light.
After hours of googling, I still need to know: Where can I find a corneal specialist who knows about this?
If this is dealt with only with lubrication and laser surgery if in the visual field, then what occurs when this degeneration degenerates? … How can I treat bad nasal symptoms (I have allergic reactions) and not get gravel in my eyes?