Diabetic Retinopathy is a medical condition with far-reaching consequences. As a serious issue linked to diabetes, it raises legitimate concerns about the long term health implications for those affected.
Definition of Diabetic Retinopathy
Diabetic Retinopathy is a diabetes complication. It affects eyes and is instigated by damage to the blood vessels of the light-sensitive tissue located at the back of the eye (retina). At first, it may start as a mild vision problem, but without proper care and timely intervention, it can eventually lead to blindness.
Causes and risk factors
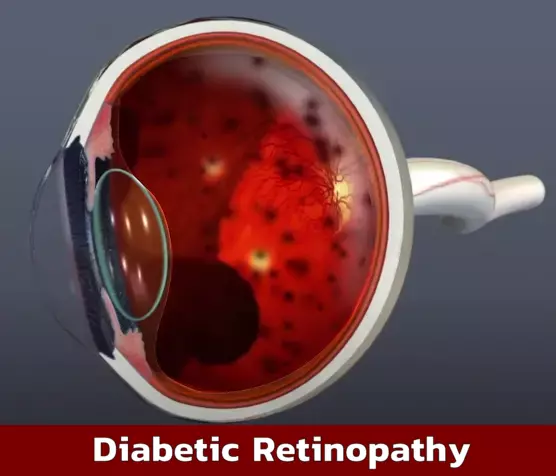
Diabetic Retinopathy is primarily caused by too much sugar in your blood leading to blockage of tiny blood vessels that nourish the retina. This can cut off blood supply, causing new blood vessels to form on the retina, which can essentially leak blood and other fluids, causing scarring and cell loss in the retina.
Risk factors can include duration of diabetes, poor control of blood sugar levels, hypertension, high cholesterol, and pregnancy.
Stages and Progression of Diabetic Retinopathy
Diabetic Retinopathy, a diabetes complication affecting eyes, usually goes through four stages, from mild to severe nonproliferative stages, to proliferative stages with advanced complications.
Mild, moderate, and severe nonproliferative stages
These stages involve the blood vessels in the retina, manifesting with few or no symptoms.
- Mild Nonproliferative Retinopathy: In this early stage, small areas in the blood vessels called microaneurysms occur.
- Moderate Nonproliferative Retinopathy: More blood vessels start getting blocked.
- Severe Nonproliferative Retinopathy: Increased blockage of the blood vessels deprives certain areas of the retina from blood supply, leading to growth signals being sent out.
Proliferative stage and advanced complications
Proliferative Diabetic Retinopathy (PDR): The advanced stage where signals sent cause growth of new blood vessels. These are abnormal and fragile. They can cause leakage into the clear, jelly-like substance in the center of your eye (vitreous). Eventually, scar tissue stimulated by the growth of new blood vessels may lead to retinal detachment or cause severe vision loss.
Common symptoms and visual changes
One might not notice Diabetic Retinopathy until it starts wreaking havoc on the vision. Key symptoms include:
- Blurry Vision: In initial stages, you might experience occurrences of blurry vision.
- Fluctuating Vision: You could experience intermittent changes in sight, at times clear, other times foggy.
- Dark Strings or Specks: Also known as floaters, they’re often precursors to bleeding from abnormal vessels.
Diagnostic tests and procedures
Catch It Early: Routinely scheduled eye examinations are the best way to detect progression, ideally before it leads to vision loss. Understanding your status comes through a series of tests.
- Fundus Photography: This involves taking images of the back of your eye, showing changes due to disease.
- Fluorescein Angiography: A dye is injected into your arm and then used to take photos in sequence as the dye passes through the blood vessels in your retina.
- Optical Coherence Tomography (OCT): Works similarly to ultrasound but it employs light waves instead of sound, generating very detailed cross-sectional images of your eyes.
Ensure regular check-ups to prevent severe complications and manage diabetes effectively.
Treatment Options for Diabetic Retinopathy
If you or your loved one has ever been diagnosed with diabetic retinopathy, you understand that it’s a severe condition that demands proactive control. However, through effective treatment and lifestyle changes, it’s possible to manage and reduce the impact of this condition.
Medical management and lifestyle changes
Blood Sugar Control: Committing to optimal blood glucose levels is essential for controlling the progression of diabetic retinopathy.
Lifestyle Changes: Complementary lifestyle changes include weight management, exercising regularly, and quitting smoking. Optimizing blood pressure and cholesterol levels can also help to slow the progression.
Surgical interventions and laser treatments
Laser Therapy: Proliferative diabetic retinopathy (PDR), a severe form of the condition, may require laser therapy. This procedure helps to slow the growth of abnormal blood vessels in the retina.
Vitrectomy Surgery: A surgical procedure called vitrectomy might be necessary when there is bleeding in the eye due to PDR, or in cases where scar tissue causes retinal detachment.
Intravitreal Injections: Anti-VEGF injections into the eye may be used to slow down the growth and leakage from abnormal blood vessels in the retina. One way or another, severe cases require more immediate medical interventions.
Prevention and Control of Diabetic Retinopathy
When we address the challenge of controlling and preventing Diabetic Retinopathy, we are talking about taking actions that prevent the progress of this damaging eye condition linked with diabetes.
Importance of blood sugar control and regular eye exams
Regulate Blood Sugar: As a matter of prevention, maintaining strict control over your blood sugar levels should be priority. Medical studies have proven that strict blood sugar control can diminish the risk of microvascular complications, including Diabetic Retinopathy.
Regular Eye Exams: Regular eye exams are crucial to early detection and treatment. They allow for early intervention before the condition progresses and leads to irreversible blindness.
Managing other risk factors
Control Other Risk Factors: Besides blood sugar control, other factors that would require management include high blood pressure and high cholesterol. These can also increase the risk of vision loss from Diabetic Retinopathy. Controlling these health conditions can further help to reduce the development or progression of this ailment.
Remember:
- Maintain strict control over your blood sugar levels
- Get regular eye exams
- Control other health conditions such as hypertension and elevated cholesterol
Your eyesight may depend on it!
Living with Diabetic Retinopathy
For those living with Diabetic Retinopathy, being aware of the disease and its impact on one’s lifestyle is paramount.
Coping strategies and support systems
Knowledge empowerment: Educate yourself about your condition; it can shape your perspective on living effectively with Diabetic Retinopathy.
Professional help: Don’t underestimate the power of professional help. Therapists and support groups can provide you with valuable insights, coping mechanisms, and emotional support.
Eye care tips and self-care practices
Regular checkups: Schedule regular appointments with your eye doctor to monitor progression and implement timely treatments.
Routine self-care: Maintain a healthy diet, regular exercise, blood sugar levels control, and adequate sleep.
Adjustment: Get comfortable with using visual aids like magnifying lenses or big-button phones. Tech companies today offer a wide range of accessibility features for visually impaired users.
In sum, living with Diabetic Retinopathy is about managing your condition wisely. By sharpening coping strategies, seeking professional help when needed, and following ongoing eye care and self-care practices, this task can be significantly easier.
Potential Complications of Diabetic Retinopathy
Every individual who has diabetes stands a risk of developing diabetic retinopathy, an eye condition that could lead to blindness if left unchecked. Despite its asymptomatic beginnings, several complications may arise over time.
Macular edema and macular ischemia
Macular Edema: This condition is characterized by the swelling or thickening of the macula – the part of the eye responsible for detailed, straight-ahead vision. This is as a result of leaking fluid from the blood vessels in the eye.
Macular Ischemia: On the other hand, macular ischemia happens when small blood vessels close up, blurring the vision due to inadequate blood flow.
Retinal detachment and vision loss
Retinal Detachment: Severe diabetic retinopathy can cause scar tissue, leading to pulling on the retina, and eventually a possible retinal detachment.
Vision Loss: The extreme consequence of all these complications is complete vision loss. It’s not immediately apparent but prolongs neglect could lead to this. Regular check-ups are crucial for early detection and treatment.



