A stye (medical term: hordeolum) develops when an oil gland at the edge of an eyelid ends up being infected. Looking like a pimple on the eyelid, a stye can grow on the within or beyond the lid.
Here are 7 things to learn about eye styes:
- The first signs are pain, redness, swelling and inflammation.
- Styes normally do not cause vision issues.
- Styes are triggered by staphylococcal bacteria.
- Styes are contagious.
- A lot of styes recover on their own.
- Never ever “pop” a stye.
- Other eye problems can accompany styes.
That’s the short variation. Discover more about symptoms, causes and treatments of a stye (sty) by reading below.
Eye styes appear as red, painful lumps which can establish whitish heads of pus like a pimple. They are not contagious so there is no risk of infection to another person. A stye is likewise called a hordeolum.
Eye Styes Symptoms
The patient will have a painful red swelling on the eyelid which can make the eye produce tears and end up being red. Often styes can look like a pimple.
Eye styes very rarely impact both eyes at the same time. A person will usually have one stye in one eye. However, it is possible to have more than one stye in the exact same eye or one in each eye.
Symptoms of an eye stye can include:
- a lump on the eyelid
- swelling of the eyelid
- pain
- soreness
- inflammation
- crusting of the margins of the eyelids
- burning feeling
- droopiness of the eyelid
- itching of the eye
- blurry vision
- discharge of mucus from the eye
- light level of sensitivity
- tearing
- discomfort when blinking
- the feeling that there is an item in the eye
The person must talk to a doctor if the stye continues for greater than 1 week, vision problems arise, if the swelling becomes especially painful, bleeds, or spreads to other parts of the face, or if the eyelid or eyes end up being red.
There are two general categories of eye stye:
External hordeolum
External styes emerge along the outer edge of the eyelid. They can become yellow, filled with pus, and painful when touched. They can be caused by an infection of the following:
- Eyelash follicle: The small holes in the skin from which eyelashes grow.
- Sebaceous (Zeis) gland: This gland is attached to the eyelash follicle and produces sebum. Sebum helps lubricate the eyelash and stop it from drying out.
- Apocrine (Moll) gland: This gland also helps avoid eyelashes from drying out. It is a gland that clears into the eyelash follicle.
Internal hordeolum
The swelling establishes inside the eyelid. Normally, an internal hordeolum is more painful than an external one. They are likewise described as an internal stye and are most commonly due to an infection in the meibomian gland. These glands are accountable for producing a secretion that makes up part of the movie that covers the eye.
Patients may likewise experience a burning experience in the eye, crusting of the eyelid margins, droopiness of the eyelids, itchiness on the eyeball, level of sensitivity to light, tearing, a feeling that something is adhered to the eye, and discomfort when blinking.
Risk factors
The following can increase the threat of establishing an eye stye:
- using cosmetics after their use-by dates
- not eliminating eye makeup prior to going to sleep
- not decontaminating contact lenses prior to putting them in
- altering contact lenses without cleaning hands thoroughly
- teenagers tend to have styes more commonly, however individuals of any age can establish them
- bad nutrition
- sleep deprivation
If a member of the family has an eye stye, the other family members should not share wash cloths or face towels to reduce cross infection.
Sometimes a sty happens as a complication of blepharitis, an inflammation of the eyelids. Blepharitis is often brought on by a bacterial infection, but can often be a complication of rosacea, an inflammatory skin problem that mainly affects the skin of the face.
Eye Styes Treatment
Most styes disappear by themselves without the requirement for any treatment. As soon as they rupture, symptoms tend to enhance rapidly.
Do not attempt to break a stye yourself.
A warm compress held carefully versus the eye may assist relieve symptoms. The water must not be too hot. Special care must be taken when applying it to someone else, such as a child.
The compress ought to be held against the eye for 5 to 10 minutes, 3 or four times each day.
Not just does the compress reduce the discomfort, but it might likewise motivate the pus to recede. When the pus has drained away, symptoms normally improve quickly.
Painkiller may be practical if the stye is particularly sore. Some are readily available for purchase nonprescription or online, such as ibuprofen or acetaminophen.
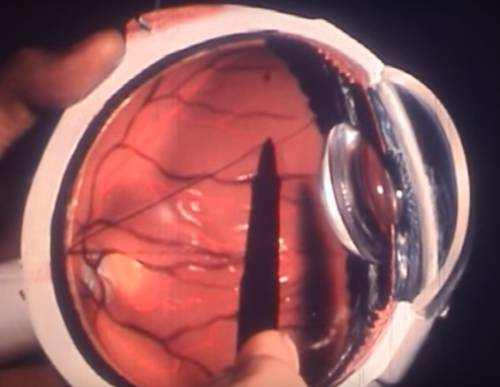
When an external stye is exceptionally painful, the doctor might get rid of the eyelash closest to it, and drain the pus away by lancing it with a thin needle. This treatment needs to only be carried out by an expert. If things do not improve, the patient may be referred to a specialist, for instance, an ophthalmologist.
If the eye stye continues, the physician might prescribe a topical antibiotic cream or antibiotic eye drops. If the infection spreads beyond the eyelid, oral antibiotics might be prescribed.
It is best not to apply eye makeup, lotions, or use contact lenses up until the stye has totally gone.
Complications Associated with Eye Styes
Complications, although exceptionally uncommon, may often take place.
These can consist of:
- Meibomian cyst: This is a cyst of the small glands located in the eyelid. The glands release a lube, called sebum in the edge of the eyelid. A persistent stye on the within the eyelid can eventually develop into a Meibomian cyst, or chalazion, especially if the gland is obstructed. This type of cyst is easily and efficiently treatable.
- Preseptal or periorbital cellulitis: This might establish if the infection spreads to the tissue around the eye. The layers of skin around the eye become irritated and red, making the eyelids go red and swollen. This is treated with antibiotics.
Although the issues can occur, as pointed out formerly, most cases of stye will clear with minimal intervention.
Facts Related to Eye Styes
1. The first signs are pain, soreness, swelling and tenderness
After symptoms appear, a small pimple will develop in the afflicted area. Typically this is accompanied by swollen eyes. In some cases simply the instant area is swollen; at other times, the whole eyelid swells.
2. Styes typically don’t cause vision problems
Your capability to see well at either near or distance should not be impacted by a stye.
3. A stye (sty) is brought on by staphylococcal bacteria
This germs is discovered in the nose and is moved easily to the eye when you rub your nose, then your eye.
4. Styes are contagious, but …
Pretty much everyone has this stye-causing bacteria in their body. We all, at any age, have the prospective to establish a stye without outdoors contamination.
Still, if you have a stye, you don’t desire the bacteria within to come into contact with somebody else’s eye. This may indeed cause them to develop a stye or other infection also. So keep your eyes and hands clean, and do not share pillowcases, bedsheets, washcloths or towels with others.

5. Many eye styes heal on their own within a couple of days
You can motivate this procedure by applying hot compresses for 10 to 15 minutes, 3 or 4 times a day, over the course of numerous days.
This will alleviate the pain and bring the stye to a head, just like a pimple. In most cases, the stye will then rupture, drain and heal without additional intervention.
6. Never “pop” an eye stye
You shouldn’t pop a style like you would a pimple. Permit the stye to rupture on its own.
A stye that forms inside the eyelid (called an internal hordeolum) may not rupture and heal by itself. Because this kind of stye can be more serious, your eye doctor may need to open and drain it.
If you have regular styes, your optometrist might want to recommend an antibiotic lotion to avoid a reoccurrence. He or she also may suggest utilizing pre-moistened eyelid cleansing pads for daily lid hygiene, to reduce the risk of styes and blepharitis.
7. Other eye issues can accompany styes
With a stye, you may observe regular watering in the affected eye, increased light level of sensitivity and a feeling like something remains in your eye (eye doctors call this a “foreign body experience”).
Chalazia: Bumps That Aren’t Styes
Frequently incorrect for a stye, a chalazion (shah-LAY-zee-on or kah-LAY-zee-on) is an enlarged, blocked oil gland in the eyelid. A chalazion mimics a stye for the first couple of days, then becomes a pain-free difficult, round bump later on.
The majority of chalazia develop farther from the eyelid edge than styes.
Although the exact same treatment used for a stye speeds the recovery of a chalazion, the bump might remain for one to numerous months. If the chalazion remains after a number of months, your eye doctor may drain it or inject a steroid to facilitate recovery.
Other Typical Eyelid Bumps
Milia. Likewise called “milk spots” or “oil seeds,” milia are tiny white cysts, typically appearing on the outer skin layer (skin) of the eyelid and around the eyes and nose. They take place when dead skin cells don’t slough off normally and are trapped at the base of a sweat gland or hair follicle, forming a raised “pinhead” bump that looks just like a whitehead.
Milia are most common in babies, but grownups likewise can be affected. In babies, milia have the tendency to clear up by themselves over a week or more, however many adults will require medical treatment.
The favored method of removing an irritating milial cyst is by a basic surgical excision (no stitch is required) by your skin doctor.
Xanthelasma. A subtype of xanthoma (zan-THOE-mah), this skin condition is characterized by yellowish bumps (plaques) under the skin, taking place on or around the eyelids.
Xanthelasma (zan-thah-LAZ-mah) typically look like disc-like lesions with a flat surface and distinct borders, ranging in size from a number of millimeters as much as 3 inches in severe cases.
They are caused by a build-up of certain fats, particularly cholesterol, under the surface area of the skin and often are attributed to raised lipid levels in the blood stream such as high cholesterol. The growth is non-cancerous, but raised blood lipids could increase your risk of heart disease and need to be investigated even more by your doctor.
Xanthelasma normally is non-symptomatic, however can be surgically gotten rid of by your doctor for cosmetic functions.
Q&A Related Eye Styes
What are the medical treatment alternatives for hordeolum (stye)?
Start treatment for hordeolum with a topical treatment. Progress to systemic therapy just if symptoms and signs of extreme infection are discovered.
What is the surgery showed for the treatment of hordeolum (stye)?
Chalazion is a chronic condition associated to hordeola and may require surgical excision. Referral to an eye doctor is suggested in all cases.
Which medications in the drug class Antibiotics are utilized in the treatment of Hordeolum and Stye in Emergency Medicine?
Antibiotics
Topical antibiotics are useful for control of staphylococcal infections in eyelids and nares.
Bacitracin ophthalmic lotion (AK-Tracin)
Prevents transfer of mucopeptides into growing cell wall; hinders bacterial cell wall synthesis.
Tobramycin ophthalmic service or ointment (Tobrex, AKTob)
Interferes with bacterial protein synthesis by binding to 30S and 50S ribosomal subunits, which leads to a malfunctioning bacterial cell membrane; readily available as option, ointment, and lotion.
Erythromycin (EES, E-Mycin, Ery-Tab)
First-choice treatment when systemic therapy is indicated; likewise indicated for treatment of infections brought on by susceptible pressures of microbes, including S aureus.
Dicloxacillin (Dycill, Dynapen)
For treatment of infections caused by penicillinase-producing staphylococci. Might be used to start treatment when a staphylococcal infection is believed.
Tetracycline (Sumycin)
Treats prone bacterial infections of both gram-positive and gram-negative organisms in addition to infections triggered by mycoplasmal, chlamydial, and rickettsial organisms; hinders bacterial protein synthesis by binding with 30S and possibly 50S ribosomal subunit( s) of prone bacteria.
Cloxacillin (Cloxapen, Tegopen)
For treatment of infections caused by penicillinase-producing staphylococci. May be used to start treatment when a staphylococcal infection is presumed.
What is the prognosis of hordeolum (stye)?
Spontaneous recovery prevails. Regular recurrences prevail. Progression to systemic infection is rare; just a couple of case reports appear in the existing literature.
When is surgical care showed in the treatment of a hordeolum (stye)?
Incision and drainage is suggested if the hordeolum is big or if it is refractory to medical therapy.
Cut and drainage is done under local anesthesia, and the incision is made through the skin and orbicularis (when it comes to external hordeola) or through the tarsal conjunctiva and tarsus (when it comes to internal hordeola). The specimen needs to be sent out for histopathological evaluation to confirm the medical diagnosis and to eliminate a more sinister pathology (eg, basal cell carcinoma).
What are the goals of drug treatment for hordeolum (stye)?
The objectives of pharmacotherapy are to deal with the infection, to lower morbidity, and to prevent problems.
How are hordeolum (stye) prevented?
Try to prevent reoccurrences by reducing or removing threat elements, such as blepharitis and meibomian gland dysfunction, through daily lid hygiene and warm compresses.