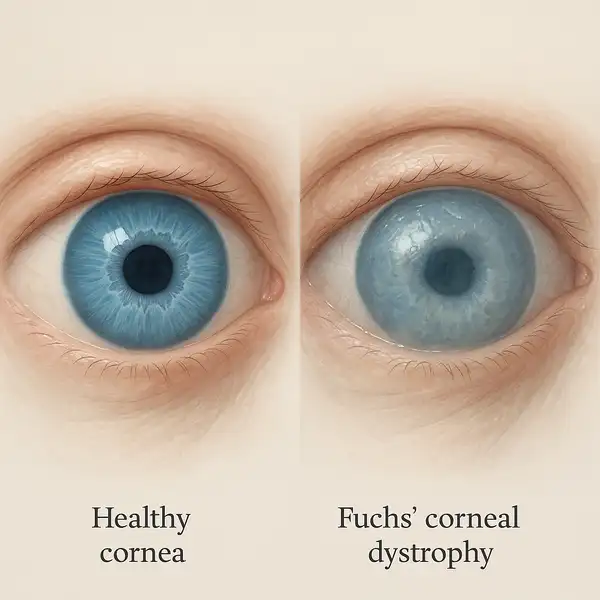
Fuchs’ corneal dystrophy is a progressive eye disease that affects the innermost layer of the cornea, called the endothelium. Over time, these cells deteriorate, leading to corneal swelling and vision problems. It typically begins to show symptoms between ages 50 and 60 but can develop earlier. Studies reveal that approximately 4% of Americans over the age of 40 are affected by some form of this condition (source: American Academy of Ophthalmology).
Prevalence of Fuchs’ Corneal Dystrophy by Age Group (2024)
| Age Group | Prevalence (%) |
|---|---|
| 30-39 years | 1% |
| 40-49 years | 3% |
| 50-59 years | 8% |
| 60-69 years | 15% |
| 70+ years | 20% |
This chart shows the increasing prevalence of Fuchs’ Corneal Dystrophy with age in 2024. The data highlights a notable rise in cases among individuals aged 50 and above, underscoring the importance of regular eye health screenings for older populations.
Early Symptoms and How They Progress
Early signs might feel like waking up with cloudy vision that clears up later in the day. Other symptoms include:
- Blurry or distorted vision: In Fuchs’ corneal dystrophy, blurriness is often most severe in the morning due to overnight corneal swelling. Unlike typical refractive errors like myopia, this blurring improves slightly throughout the day as the swelling diminishes.
- Sensitivity to light (photophobia): Patients often report intense glare sensitivity, especially to headlights and sunlight. This symptom is more persistent and irritating compared to the light sensitivity seen with dry eye syndrome.
- Gritty sensation in the eyes: While dry eye disease also causes grittiness, in Fuchs’ dystrophy it is specifically linked to epithelial edema (fluid buildup in the cornea), making the sensation deeper and more constant rather than intermittent.
- Poor night vision: Difficulty seeing in low light is common but, in Fuchs’ patients, it is compounded by corneal haze and distorted light scattering, which can cause halos and starbursts around lights—symptoms that worsen over time and are more disabling than standard “night blindness” seen in aging.
As the disease advances, these symptoms worsen and may lead to significant visual impairment. Everyday activities like driving, reading, and even recognizing faces can become increasingly difficult, causing understandable frustration.
Causes and Risk Factors
Fuchs’ corneal dystrophy can be inherited (thanks, genetics!) or occur without a family history. Factors increasing the risk include:
- Family history of the disease: Around 50% of individuals diagnosed with Fuchs’ corneal dystrophy report a family history, making it a significant risk factor. Genetic predisposition can be triggered earlier by oxidative stress or environmental damage.
- Being female (women are 2-3 times more likely to develop it): Women account for nearly 70% of cases. Hormonal fluctuations, particularly during menopause, may exacerbate endothelial cell degeneration.
- Having diabetes: Approximately 20% of Fuchs’ patients also have diabetes. Chronic high blood sugar levels can cause microvascular damage and oxidative stress, accelerating endothelial cell loss.
- Exposure to UV light without protection: Long-term, unprotected UV exposure increases the risk by up to 30%. UV radiation induces oxidative stress and inflammation in corneal tissues, promoting earlier onset and faster progression of the disease.
Genetic mutations in the COL8A2 and TCF4 genes have been implicated in familial cases, adding a molecular twist to the understanding of this condition.
How Fuchs’ Corneal Dystrophy Is Diagnosed
Eye doctors have a variety of cutting-edge tools for diagnosis:
| Diagnostic Method | How It Works | Accuracy (1-10) | Average Cost (USD) |
|---|---|---|---|
| Slit-lamp examination | Magnified view of the cornea to spot abnormalities | 8 | $100-$200 |
| Specular microscopy | Photographs endothelial cells to measure health | 9 | $200-$400 |
| Optical coherence tomography (OCT) | High-res imaging of corneal layers | 10 | $300-$600 |
| Pachymetry | Measures corneal thickness (swelling indicator) | 8 | $150-$300 |
Each of these methods offers unique advantages, and many ophthalmologists use a combination for a foolproof diagnosis.
Diagnosis Methods for Fuchs’ Dystrophy Used by Ophthalmologists (2024)
The chart outlines the diagnostic methods employed by ophthalmologists in 2024 for identifying Fuchs’ Dystrophy. Slit-lamp examination remains the most widely used method, while genetic testing is less common but growing in importance.
Modern Treatments: What’s New?
Today’s treatments for Fuchs’ are pretty cutting-edge, not your grandma’s remedies!
Medications
- Hypertonic saline eye drops (e.g., Muro 128): These drops work by drawing excess fluid out of the cornea, thereby reducing swelling and improving clarity. Patients typically use them four to six times a day, especially upon waking when swelling is most pronounced.
- Topical antioxidants: Currently under active research, these compounds aim to slow the oxidative damage responsible for endothelial cell death. While not yet commercially available, early clinical trials show promising results for extending the lifespan of remaining healthy cells.
- Rho-kinase inhibitors (e.g., Ripasudil): These experimental eye drops help stimulate endothelial cell proliferation and migration. They are often prescribed following surgical procedures like DSO to enhance healing and improve overall outcomes.
Surgical Innovations
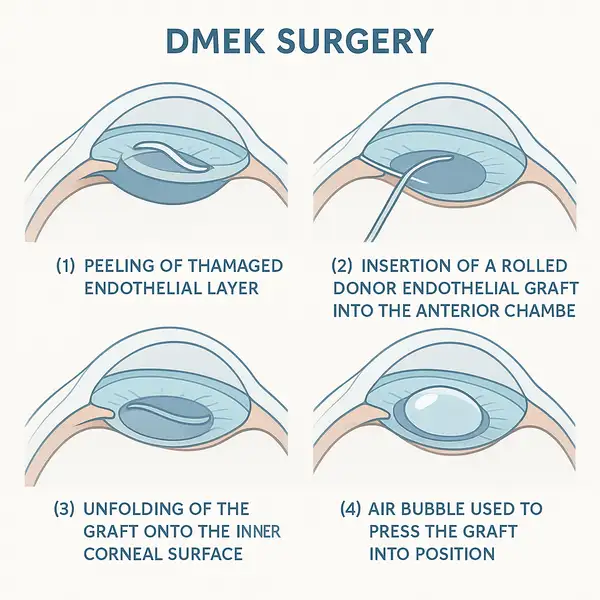
- Descemet Membrane Endothelial Keratoplasty (DMEK):
- This advanced microsurgical technique selectively replaces only the damaged endothelial layer, preserving much of the natural cornea.
- Patients typically experience rapid visual recovery within 4-6 weeks, with the majority achieving 20/25 vision or better.
- Success rate: 95% (source: American Society of Cataract and Refractive Surgery).
- Average cost for DMEK surgery ranges from $7,000 to $12,000 depending on the facility and geographic location.
- Fun fact: DMEK has the lowest rate of rejection among all corneal transplant procedures!
- Descemet Stripping Only (DSO):
- In this newer procedure, surgeons carefully remove only the central diseased endothelial cells without any donor tissue replacement.
- Recovery is aided by the natural migration of peripheral healthy endothelial cells.
- When paired with Rho-kinase inhibitors, the healing process can be significantly accelerated, reducing the need for further intervention.
- Best suited for early to moderate stages of Fuchs’ dystrophy where enough healthy cells remain.
- Artificial corneas (keratoprosthesis):
- An alternative for patients with severe disease, multiple failed transplants, or other complicating factors.
- These synthetic implants are engineered to permanently replace the cornea, providing a clear optical path.
- Costs can run between $15,000 and $30,000, covering preoperative evaluations, surgery, and extensive postoperative care.
- Patients must adhere to strict postoperative monitoring to prevent infection, glaucoma, or extrusion of the device.
Real Medical Cases
- Male, 59, Chicago, IL: A retired engineer first noticed worsening halos and glare while driving at night, describing it as “looking through a fogged-up window.” After months of progressive blurring and morning haziness, he sought evaluation and was diagnosed with Fuchs’ dystrophy. He underwent DMEK surgery at a leading Chicago eye center. Just eight weeks post-operation, he reported “almost perfect vision” and comfortably returned to activities like golfing, woodworking, and reading fine print, regaining a huge part of his independence.
- Female, 45, Miami, FL: A graphic designer went for a routine eye exam after experiencing mild morning blur and occasional discomfort that was impacting her ability to distinguish subtle color changes on screens. Specular microscopy revealed early Fuchs’ changes. She began daily use of hypertonic saline drops (Muro 128), installed a home humidifier, upgraded her workspace with moisture-retaining indoor plants, and started wearing wraparound sunglasses even on overcast days. Thanks to these interventions, she continues to manage her condition effectively and maintains her full-time design career.
Practical Table: Managing Fuchs’ Daily
| Tip | How It Helps |
|---|---|
| Use a humidifier | Reduces eye dryness |
| Wear UV-blocking sunglasses | Protects corneal cells |
| Schedule regular eye exams | Early intervention = better outcomes |
| Avoid over-the-counter redness drops | Can worsen swelling |
| Take screen breaks every 20 minutes | Reduces ocular surface stress |
Editorial Advice
“Early diagnosis is your ticket to keeping great vision,” says Reyus Mammadli, healthcare advisor. “Modern surgical options, especially DMEK, are game-changers. Patients shouldn’t wait for severe symptoms to appear before seeking help.”
Patient Satisfaction with Fuchs’ Dystrophy Treatments (Survey 2024)
| Satisfaction Level | Percentage (%) |
|---|---|
| Highly satisfied | 48% |
| Satisfied | 34% |
| Neutral | 10% |
| Dissatisfied | 6% |
| Highly dissatisfied | 2% |
This chart summarizes patient satisfaction levels with treatments for Fuchs’ Dystrophy based on a 2024 survey. A majority of patients reported being highly satisfied or satisfied, reflecting positive outcomes and overall treatment effectiveness.
Additionally, the editorial team recommends being proactive about eye protection, maintaining a moist indoor environment, and following up diligently with an eye care provider. If you notice subtle changes in your vision, don’t brush it off—catching Fuchs’ early can make all the difference!
References
- American Academy of Ophthalmology. Fuchs’ Corneal Dystrophy Overview. Retrieved 2024.
- American Society of Cataract and Refractive Surgery. Corneal Transplant Innovations. Retrieved 2024.
- Cornea Society. Updates on Endothelial Cell Research. Retrieved 2024.
- National Eye Institute. Facts About the Cornea and Corneal Disease. Retrieved 2024.
- Mayo Clinic. Fuchs’ Dystrophy: Symptoms and Causes. Retrieved 2024.



