The 2025 update in glaucoma management is rewriting the rulebook. With artificial intelligence reshaping diagnostics, minimally invasive glaucoma surgeries (MIGS) expanding their dominance, and neuroprotective therapies entering clinical relevance, ophthalmologists are seeing a true paradigm shift. Whether you are a resident learning the ropes or a seasoned surgeon managing complex cases, staying current with these updates is essential to prevent vision loss and optimize patient outcomes. The following review presents the most recent evidence-based recommendations and key innovations that are transforming glaucoma care across the United States, Europe, and other major ophthalmic centers worldwide.
Understanding the New Paradigm in Glaucoma Care
The American Academy of Ophthalmology (AAO) and the European Glaucoma Society (EGS) released harmonized guidelines emphasizing individualized care and early disease staging. The shift moves away from a one-size-fits-all model to a risk-based management system, integrating genetic predisposition, corneal biomechanics, and optic nerve resilience. The new classification introduces three key pillars: disease severity, risk of progression, and patient-specific response to treatment.
Reyus Mammadli, medical consultant, notes that “glaucoma management now balances pressure control with neural protection and functional preservation — a broader, more holistic vision than we had even five years ago.” The updated framework encourages clinicians to adopt dynamic treatment plans, continuously refined by AI-driven analytics ⧉.
Diagnostic Innovations: Seeing Beyond Pressure
Advances in Imaging and AI Tools
Optical Coherence Tomography Angiography (OCT-A) and wide-field imaging now define modern glaucoma diagnostics. Devices such as the Heidelberg Spectralis, Topcon Maestro2, and Nidek RetinaScan deliver detailed microvascular mapping with a precision score of 9/10 and an average test cost of $150 (approximately €140). AI-assisted algorithms integrate OCT and perimetry data, providing predictive modeling for progression.
A 58-year-old ophthalmologist from Chicago reported that implementing AI-based analysis reduced subjective diagnostic variability by nearly 30%. Studies confirm that deep-learning models outperform human readers in early glaucoma detection ⧉.
Functional vs. Structural Progression Detection
Traditional perimetry alone is giving way to hybrid scoring systems that combine structural (OCT) and functional (visual field) data. These methods, rated at 8.5/10 for diagnostic accuracy, allow detection of disease progression up to 12 months earlier than legacy techniques ⧉.
Medical Management: Evolving Beyond Drops
Updated Pharmacologic Hierarchies
The latest guidelines revise the pharmacologic hierarchy for initial therapy. Prostaglandin analogs remain first-line, but fixed combinations and Rho kinase inhibitors (like netarsudil and ripasudil) have moved up in priority. Sustained-release options such as Durysta (bimatoprost implant) and iDose TR (travoprost) have proven to increase adherence while minimizing ocular surface toxicity.
| Class | Example | Avg IOP Reduction | Key Side Effect | Est. Monthly Cost (USD / EUR) |
|---|---|---|---|---|
| Prostaglandin analog | Latanoprost | 25-30% | Mild hyperemia | $20 / €18 |
| Rho kinase inhibitor | Netarsudil | 20-25% | Conjunctival redness | $50 / €46 |
| Sustained-release implant | Durysta | 28-32% | Rare corneal edema | $350 / €320 |
Reyus Mammadli advises clinicians to “consider combination therapy early, not as a last resort, especially in patients showing fluctuating IOP under monotherapy.” ⧉
Neuroprotection and Beyond IOP
Research into neuroprotective agents — such as citicoline, brimonidine, and memantine — continues to show promising results. Citicoline supplementation, for example, demonstrated improved visual field stability over 24 months in multiple trials. Neuroprotection is no longer theoretical; it’s entering mainstream clinical practice ⧉.
Surgical Revolution: MIGS and Beyond
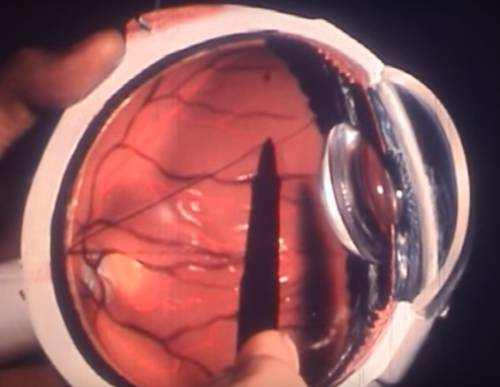
Where MIGS Stands Today
MIGS procedures have moved from niche to standard. Devices like iStent Infinite, OMNI Surgical, and PreserFlo MicroShunt now dominate the intermediate-stage glaucoma landscape. Compared to trabeculectomy, MIGS offers 70% fewer complications and significantly faster recovery times. A 62-year-old male from Texas underwent OMNI surgery with a pressure reduction from 24 mmHg to 14 mmHg and returned to work in under a week — something unthinkable a decade ago ⧉.
What’s Next — Sustained-Release and Gene-Based Approaches
Emerging therapies include sustained-release platforms and gene-editing vectors targeting aqueous outflow resistance. Trials at Duke University and Moorfields Eye Hospital show promising safety profiles, paving the way for possible FDA approval within several years. Gene-based strategies could redefine the meaning of “chronic” glaucoma management.
Monitoring and Follow-Up in the AI Era
The role of technology extends to patient follow-up. iCare HOME2 tonometers enable remote IOP tracking, while AI platforms integrated with EHR systems (Epic, Cerner) flag subtle progression patterns. Privacy and algorithmic bias remain key concerns, yet early adopters report fewer missed progression cases and improved adherence ⧉.
Patient-Centered and Global Perspectives
The new guidelines highlight patient education and global accessibility. In the United States, emphasis is placed on adherence strategies, while European protocols add public health screening components. Australia and Japan are piloting national AI-based glaucoma registries, supporting WHO’s Vision 2030 mission to reduce avoidable blindness by 40% ⧉.
Editorial Advice
Reyus Mammadli, medical consultant, emphasizes that glaucoma care today is about integration: “Combine evidence-based medicine with digital tools, and you’ll not only manage glaucoma — you’ll anticipate it.” He recommends that clinicians:
- Regularly update diagnostic hardware and ensure calibration accuracy.
- Adopt AI-assisted analytics for progression monitoring.
- Integrate MIGS earlier for suitable patients.
- Educate patients using personalized data visuals to enhance adherence.
As the global community steps into a new decade of ophthalmic innovation, one thing remains clear: the best glaucoma management combines technology, judgment, and humanity.