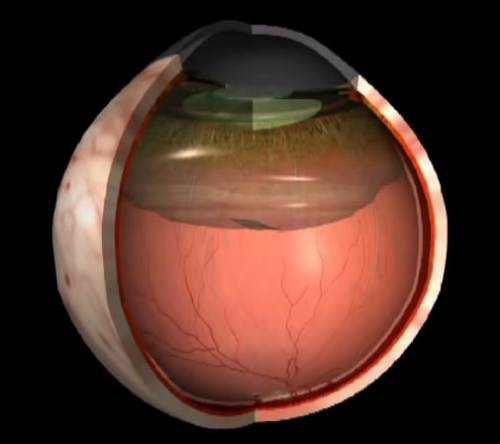
Posterior Vitreous Detachment definition: Posterior Vitreous Detachment (PVD) is a natural modification that takes place in older adults, when the vitreous gel that fills the eye separates from the retina, the light-sensing nerve layer at the back of the eye.
Symptoms of Posterior Vitreous Detachment
- Floaters (mobile blurry shadows that obscure the vision).
- Flashes (streaks of light, typically at the side of the vision).
These symptoms generally become less extreme over numerous weeks. Many patients experience PVD after age 60, once in each eye, and the condition is usually non-sight-threatening however occasionally affects vision more completely in case of issue, such as retinal detachment or epiretinal membrane.
Mild floaters in the vision are normal, however a sudden increase in floaters is frequently the first symptom of PVD.
During posterior vitreous detachment, floaters are often accompanied by flashes, which are most obvious in dark environments. The majority of patients experience floaters and flashes during the first couple of weeks of a PVD, however sometimes the symptoms are hardly noticeable. If PVD is complicated by vitreous hemorrhage, retinal detachment, epiretinal membrane, or macular hole, the flashes and floaters may be accompanied by decreased or distorted vision. Floaters are most annoying when near the center of vision and less annoying when they settle to the side of the vision. They may appear like cobwebs, dust, or a swarm of insects– or in the shape of a circle or oval, called a Weiss ring.
Causes of Posterior Vitreous Detachment
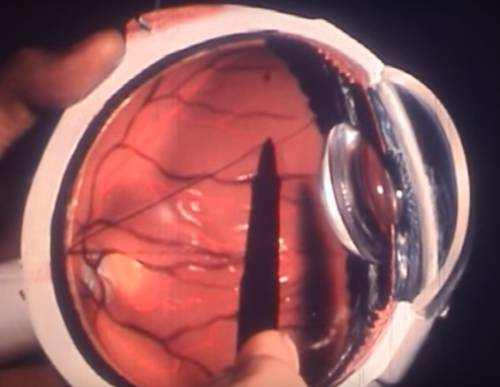
With time, the vitreous gel that fills the eye becomes liquid and condenses (shrinks) due to age and normal wear and tear. Eventually it can not fill the entire volume of the eye’s vitreous cavity (which remains the same size during their adult years) therefore the gel separates from the retina, located at the extremely back of the eye cavity.
Over the next 1 to 3 months, the vitreous gel further condenses and the sides of the gel likewise different from the retina up until the PVD is complete and the vitreous gel is attached to the retina only at the vitreous base. Clear vitreous fluid fills the space between the condensed vitreous gel and the retina.
If a PVD progresses carefully, slowly, and uniformly, the symptoms are usually mild. Nevertheless, if the forces of separation are strong or concentrated in a particular part of the retina, or if there is an abnormal adhesion (sticking together) between the vitreous gel and the retina (such as lattice degeneration), the PVD can tear the retina or a retinal blood vessel.
Flashes and floaters are generally more apparent when PVD is complicated by a retinal tear or vitreous hemorrhage. These conditions can cause additional complications, such as retinal detachment or epiretinal membrane, which can result in long-term vision loss. Nevertheless, about 85% of patients who expe- rience PVD never establish complications and for the most parts, the flashes and floaters go away within 3 months.
Risk Factors
Posterior vitreous detachment is uncommon in people under the age of 40, and progressively common during sophisticated age.
Extra risk factors for PVD consist of myopia (nearsighted- ness), trauma, and current eye surgery such as a cataract operation. Patients who experience PVD in one eye will often experience PVD in the other eye within 1 year.
Diagnosis
Posterior vitreous detachment is typically diagnosed with a dilated eye evaluation. Nevertheless, if the vitreous gel is very clear, it may be hard to see the PVD without extra testing, such as optical coherence tomography (OCT) or ocular ultrasound.
Treatment for Vitreous Detachment
PVD is non-sight-threatening and the symptoms subside in the huge majority of patients. A lot of patients not see flashes or floaters 3 months later, and no treatment or further check- ups are required at that time. Complications of PVD are uncommon however can be severe and require urgent treatment, such as laser for a retinal tear or surgery for a retinal detachment. For this reason, several checkups are suggested within 3 months after the start of PVD. Seldom, the floaters from PVD continue, and vitrectomy surgery to remove the floaters works; you and your doctor may consider this after discussing the risks and advantages of surgery.