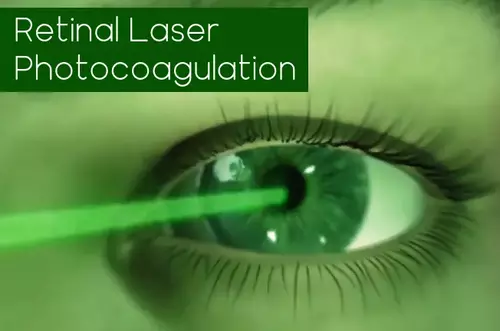
Surgery to strengthen the retina is called laser photocoagulation. Using special equipment, an ophthalmic surgeon sends a laser beam into the patient’s eye and “seals” the problem area.
The retina is the main element of the structure of the organs of vision, a sensitive membrane that covers the entire inner cavity of the eye. It makes it possible to perceive light impulses. Moreover, the retina is a kind of mediator, which ensures the interaction between our optical system and the visual sections of the brain. In other words, it is the retina that receives, processes and transmits visual information.
Possible problems with the retina should be considered if the vision significantly deteriorates within a short period of time. Double vision, blurred or indistinct pictures, strange “sparks”, “gnats” or “sand”, as well as dizziness and migraines should be reasons for an immediate visit to the doctor.
One of the most common diseases of the retina is retinal dystrophy. This is the destruction of retinal tissue. The risk group includes not only elderly people but also those who have had eye or head trauma or suffer from vascular diseases of a system nature.
See also: Parts of the Eye and What They Do
Why does a retinal dystrophy develop and what may it cause?
Various factors may lead to dystrophic changes in the retina. For example, the process of tissue scarring may start due to the disturbances in the vascular system of the organs of vision or the general immune system. Many specialists link the development of dystrophic phenomena with an unbalanced diet and bad habits, in particular smoking and alcohol abuse. The retina may also suffer from viral diseases if the patient is not provided with timely and qualified medical care.
Diabetes mellitus, high blood pressure, heart diseases, and metabolic disorders may also lead to dystrophic changes of the retina.
If a patient has been diagnosed with retinal dystrophy, he needs immediate medical assistance. Otherwise, serious complications may develop, including retinal detachment.
The onset of retinal detachment may be evidenced by the so-called “photopsia”, the appearance of “flashes”, “sparks” and “lightning” before the eyes. You should also pay attention to “flies” in front of the eyes in conjunction with the so-called “Weiss ring” – a cloudy area of circular outlines. The beginning of retinal detachment may be evidenced by the constant “shroud” in front of the eyes, rapid deterioration of vision, distortion of the outlines of objects and their size.
Retinal detachment usually begins at the periphery but with time affects the center of the retina, resulting in complete loss of vision. That is why it is necessary to take measures even at the first signs of retinal degeneration. Most often, physicians recommend laser photocoagulation.
Laser photocoagulation has recently become an increasingly popular surgical intervention. This procedure is primarily of preventive value because it helps prevent the rupture or detachment of the retina in the case of retinal dystrophy, and also improves the blood flow and increases visual acuity. At this moment coagulation is recognized as one of the most effective procedures for the treatment of retinal diseases.
Indications for Retinal Laser Photocoagulation
Retinal Laser Photocoagulation is indicated for many diseases of the eye.
- In case of hereditary or acquired retinal dystrophy which affects the photoreceptor cells. To prevent the development of peripheral detachment of the retina which is often caused by dystrophy, problematic zones are “sealed” by laser.
- In case of vascular diseases of the organ. For example, the procedure helps prevent the so-called neovascularization – in other words, vascular overgrowth.
- In retinopathy – the appearance of local areas of thinning of the retinal layer. This may be due to a variety of reasons, but usually it does not manifest itself in adult patients. Nevertheless, retinopathy may later on lead to ruptures which is why experts often recommend laser photocoagulation in such cases.
- Retinal detachment. It usually develops due to other diseases, but it is considered as a separate serious problem.
Now let’s talk about retinal laser photocoagulation benefits and risks:
Retinal Laser Photocoagulation Risks
Just like any other surgery, laser photocoagulation has its contraindications and the procedure is categorically not recommended or should be postponed to a later date.
In case of cataract and other diseases that impair transparency of the eye medium, an ophthalmologist may simply not be able to see the affected areas clearly. Therefore, before laser photocoagulation, the underlying disease should be treated first.
If the retinal detachment is advanced, the procedure is useless, which is why laser photocoagulation is not performed. Hemorrhages (hemorrhages) can also be a serious hindrance to coagulation because they prevent the ophthalmic surgeon from seeing the problem areas. If the hemorrhage is a one-time hemorrhage, the procedure is performed after the blood has resolved.
Finally, with grade III or higher gliosis, when the light-sensitive cells of the retina are replaced by connective tissue, coagulation simply does not help solve the problem, so there is little point in performing it.
It is noteworthy that pregnancy is not an absolute contraindication for laser photocoagulation. Patients can undergo the procedure practically until they give birth. Moreover, some women are recommended to undergo it if they decide to give birth naturally, without resorting to caesarean section. In this case, the risk of retinal ruptures increases with labor, so coagulation is an effective prophylaxis. Of course, patients should consult a gynecologist before the procedure.
Retinal Laser Photocoagulation Benefits
Laser coagulation is performed as an outpatient procedure. No special preparation is required. The procedure is non-contact, and therefore bloodless, and also does not require a long time (one session lasts a maximum of twenty minutes). Since local droplet anesthesia is used, anesthesia is not a burden on the patient’s internal organs and systems. Just a few hours after the operation, the patient can return to normal activities, with only minor time limitations.
How does the surgery go?
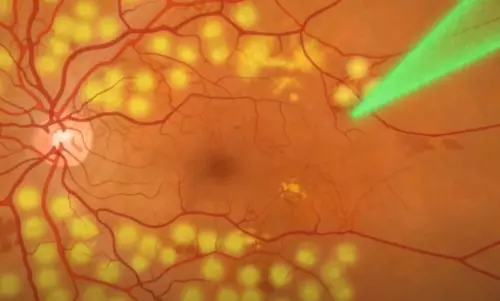
Laser photocoagulation is based on the application of the argon laser beam on a limited zone of the retina. Under their influence, a local temperature increase occurs in this area which results in tissue coagulation (clotting). This process is very fast and does not cause haemorrhages; the treated sections are literally “soldered” to the eye vasculature.
Laser photocoagulation
procedure
The procedure is performed under local droplet anesthesia in a sitting position. The patient’s eye is immediately injected with anesthetic and pupil dilating drops which ensures adequate access even to the most hard-to-reach areas of the retina.
Good to know: Side Effects of Eye Dilation
The patient is then fitted with a special lens on the eye, which allows laser radiation to enter the eyeball and focus specifically on the problem area. At this stage the patient may feel slight discomfort. It is important to note that the lens also reliably fixes the eye to prevent the laser beam from reaching the healthy retina.
The surgeon controls the intervention through a stereomicroscope. Coagulation may be performed in limited areas of the retina or circumferentially – depending on the indication in each case. In the course of the procedure, the argon laser heats the surface of the retina, “gluing” it to the vascular bed. The coagulation points act as “nails” which keep the tissue from rupturing and detachment. In total, the doctor can perform up to three hundred cauterizations.
The patient himself will see the laser action as bright flashes of light. As a rule, patients do not feel any discomfort, although some complain of tingling, attacks of dizziness and nausea. After the surgery is completed, the doctor removes the lens. The patient has to sit quietly for a few minutes to recuperate.
See also: Eye Correction Surgeries
Retinal Recovery after Laser Photocoagulation
For a certain period of time after surgery the effects of pupil dilating drops will persist. If coagulation was performed on only one eye, it will have practically no effect on your vision. Nevertheless, even in this case you should be careful not to engage in activities that require attention and quick reaction time before the pupil returns to normal.
Depending on which particular hospital, private or public, performed the surgery, the patient may leave the medical facility either immediately or after a few days. Generally, the second option is preferable, because the doctor will be able to check the condition of the retina on a daily basis, monitoring the healing process. The nurse will also administer any necessary medications.
Most private clinics allow patients to leave the institution just a few hours after laser photocoagulation. Specialists recommend to go home in two-three hours, when the normal visual acuity is completely restored. Moreover, it is always better to ask your friends and relatives to pick you up from the clinic.
As a rule, in most cases, during the first hours after surgery, you will develop some swelling and redness. These symptoms are considered quite normal and go away on their own.
The retina recovers completely in about two weeks. During this period, it is advisable to observe a number of restrictions. In particular, avoid activities that involve vibration, shaking, or the possibility of falling. Reduce eye strain to a minimum, spend as little time as possible in front of the computer. Do not drink or smoke and avoid other stimulants. Do not visit a bathhouse, a solarium, or a sauna. Do not lift heavy weights or subject yourself to serious physical exertion. Finally, do not bend over or sleep with your feet above your head.
It is extremely important to avoid colds, as the operated eye is highly vulnerable to any inflammatory processes. During this period, it is best to avoid visiting public places.
Complications and consequences
As any surgical intervention, retinal photocoagulation can cause complications. One of the most widespread negative consequences is conjunctival inflammation. Preventing it is easier than curing it, which is why it is recommended to use certain drops immediately after coagulation. If the inflammatory process does begin, antibiotics are used.
It is also common to see retinal detachment repeatedly. This happens if the procedure has not helped to eliminate the underlying cause of the disease. If relapse occurs, the same method is used – repeated laser photocoagulation.
Sometimes surgery can provoke a variety of visual impairments. These can develop immediately – and in this case go away after the swelling goes down – or they can start after a while. The patient may complain of a narrowed field of vision, spots or dots in front of the eyes. In this case, immediate medical attention is necessary.
Some patients complain of “dry eye syndrome” which occurs after the surgery due to insufficient tear fluid production. As a result, the patient feels burning and discomfort. This can be treated with special eye drops.
See also: Best OTC Eye Drops
Other types of complications are extremely rare. Usually they are not caused by the effect of the laser beam, but by the fact that the underlying disease is progressing. Therefore it is recommended to visit an ophthalmologist at least once a year. Periodic examination of the eye fundus is also indicated.



